
Addressing Canada’s ability to respond to public health emergencies has emerged as a top policy priority in the aftermath of SARS and given the current threat of an avian flu pandemic. The management of the SARS outbreak clearly demonstrated critical problems with this country’s capacity and governance structures in responding to public health emergencies. Public health reform in response to SARS has largely focused on developing collaborative intergovernmental relationships that can be relied upon in the event of an emergency.
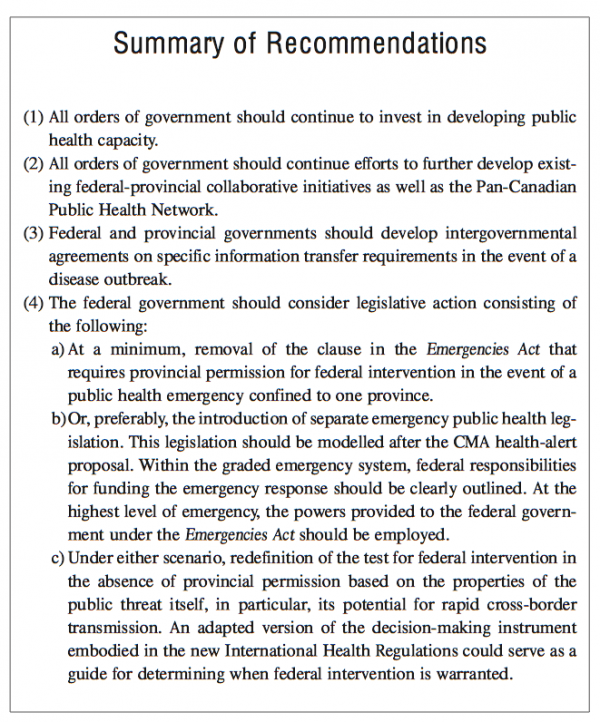
In this study, Kumanan Wilson, MD, and Harvey Lazar argue that some of the emergency response problems that were highlighted in the reports examining the SARS outbreak remain unresolved. In particular, there are important limitations in the current federal legislative framework to address emergencies, which impede the federal government’s ability to act at the early stage of an outbreak. They argue that legislative reform to provide the federal government with the freedom to act on an outbreak that is initially within the confines of only one province but is potentially of national concern should be a priority.
While an amendment to the Emergencies Act may achieve this goal, a better option, according to the authors, would be to create separate public health emergency legislation. This legislation should, first, authorize federal intervention when an emergency can be reasonably assumed to pose a national threat; second, provide increasing federal power in accordance with the gravity of the threat; and finally, ensure that the use of federal power does not create an undue financial burden for provincial governments. They believe that appropriately designed legislation will (1) allow the federal government to intervene at an early stage when the ability to control an outbreak is at its greatest; (2) ensure that the federal government has full information on the outbreak that it can then communicate to the other provinces so that they can adequately prepare; and (3) allow Canada to meet its reporting obligations as outlined in the new International Health Regulations. This legislation would, however, only serve as a contingency plan since, ideally, existing collaborative intergovernmental relationships will work effectively in a time of crisis. Nevertheless, say the authors, the policy course they recommend would ensure that agencies responsible for public health at all levels of government are protected from the effects of problems in intergovernmental relations that may occur in other policy areas and that could undermine federal, provincial and local cooperation in combatting a developing epidemic.
Public health renewal has emerged as an important policy issue in Canada, largely in response to the outbreak of severe acute respiratory syndrome (SARS) in Toronto in 2003 and in preparation for a possible avian flu pandemic. Of particular concern has been the capacity of this country to respond to public health emergencies in a rapid, coordinated and effective manner. In attempting to address this issue, the federal government has chosen to take a largely collaborative approach with the provinces, on the assumption that effective relations between orders of government can be maintained in the event of an emergency (Wilson 2004). In doing so, Ottawa is choosing not to adopt new legislation that could provide the federal government with the additional authority that might be needed in the event that intergovernmental relations turn out to be unsatisfactory during a crisis.
This article will explore some of the policy options available to the federal government when considering its role in responding to public health emergencies. An integral part of the public health renewal process will be to better define federal jurisdiction and responsibilities in the event of a public health emergency. At present there remains some uncertainty in this regard, the consequences of which could be considerable in the event of a major new infectious threat. We argue here that a redefinition of federal capacity to respond to public health emergencies must be a priority of the current legislative renewal process. We believe that amendments to the current Emergencies Act — or the creation of separate emergency public health legislation — that take into consideration unique aspects of public health emergencies should be a top priority in this country’s efforts to ready itself to respond to the next pandemic threat.
Public health is defined as what we “as a society, do collectively to assure the conditions for people to be healthy” (Institute of Medicine 1988, 19). There are several components of public health, including health promotion, health protection, disease prevention and emergency preparedness. A variety of recent threats have focused Canadian policy-makers’ attention on the health protection and disease prevention components of public health as they relate to infectious disease in particular. These include the discovery of bovine spongiform encephalopathy (“mad cow disease”), the emergence of West Nile virus, the threat of bioterrorism and the impact of SARS. While we focus in this paper on the governance responses to these threats, and to SARS in particular, it is essential to recognize that, while governance is critical to effectively managing an emerging infectious disease outbreak, of equal if not greater importance is the development of appropriate public health capacity. It became apparent from Canada’s response to SARS that the current public health infrastructure in this country considerably limited our ability to respond effectively to the threat. There is a general recognition that public health requires an infusion of funds to train more public health personnel; to enable research, investigation and knowledge translation; to better equip public health centres; and to improve surveillance infrastructure. Having highly effective public health governance structures in place is of negligible effect if adequate public health personnel are not present to carry out the core ground level public health functions.
Conversely, the efforts of public health personnel at the ground level could be wasted if governance structures are not in place to ensure responses are coordinated and comprehensive. Canada’s response to the outbreak of SARS clearly demonstrated the crucial need for effective governance to manage an outbreak, while exposing some of the limitations of the governance structures that existed at the time. The details of the management of the outbreak have been well described in several reports (Goel 2004). To summarize, SARS was originally identified as a case of atypical pneumonia in Guangdong province in China in November 2002. In February 2003, the first Canadian case arrived in Toronto, sparking an outbreak that eventually affected 438 individuals and resulted in 44 deaths. The outbreak also had a substantial negative impact on the economy of Toronto, partly due to an advisory issued by the World Health Organization recommending against travel to the city (World Health Organization 2003b; Svoboda et al. 2004). Managing the spread of SARS presented a considerable challenge to all orders of government, largely because of a lack of knowledge about several critical aspects of the pathogen, including its level of infectivity and the exact mode of its transmission (Wenzel and Edmond 2003). In Toronto, the initial management of the outbreak occurred at the hospital and local public health levels in the areas where the disease first appeared. The provincial government soon became involved and declared the situation an emergency, allowing the government to employ aggressive protective measures such as quarantine (Mackay 2003).1 Among the federal government’s responsibilities in the management of SARS was providing epidemiologic and laboratory support to provincial and local officials; managing issues related to the spread of the disease at international borders; and communicating information on the status of the outbreak to other provinces, international organizations and other nations (National Advisory Committee on SARS and Public Health 2003, chap. 2).
While there were many successes in the management of SARS at local, provincial, national and international levels, much attention has been focused on how management of the outbreak could have been improved. In particular, policy-makers and academics have examined the role of the federal government in outbreak response. When considering mechanisms by which the federal government could have involved itself to a greater extent in Ontario, it soon becomes apparent that there are real limitations on Ottawa’s power to act unless it has the consent of the affected province. The federal government’s ability to act in a public health emergency is largely governed by two pieces of legislation: the Emergencies Act2 and the Emergency Preparedness Act.3 The Emergency Preparedness Act primarily serves as companion legislation to the Emergencies Act, and provides authority for the provinces and federal government to act collaboratively to prepare for an emergency. On the other hand, the Emergencies Act, which replaced the federal War Measures Act in 1985, provides the federal government with authority to take action to address a “national emergency.” Under this Act an infectious outbreak (disease in human beings, animals or plants) is one of several categories of emergency considered as a “public welfare emergency.” Others include accidents, pollution and natural disasters. The Emergencies Act confers substantial powers on the federal government to control public welfare emergencies. These include the regulation of travel to the affected region, evacuation of the area, possession of property and the direction of services to provide emergency care. In general these would be considered adequate powers to manage an infectious outbreak. However, the Act also provides an important limit on federal power, by specifically stating that:
The Governor in Council may not issue a declaration of a public welfare emergency where the direct effects of the emergency are confined to, or occur principally in, one province unless the lieutenant governor in council of the province has indicated to the Governor in Council that the emergency exceeds the capacity or authority of the province to deal with it.4
It appears to us that the single-province constraint in the existing emergency legislation has more applicability to accidents and natural disasters, which by their nature are likely to be confined to a single geographic area. It is much less obvious that the federal government should be similarly constrained in the case of an infectious disease outbreak. According to the existing legislation, the federal government must ask permission before being allowed to take action to control a disease outbreak that has occurred in only one province. The implications of this limitation to federal powers were evident in the management of SARS, which in Canada was primarily confined to Ontario although it was present in 26 other countries.5 By not having the necessary authority, the federal government was dependent on provincial cooperation for information on the nature and extent of the outbreak. It soon became evident that cooperation between the provincial and federal governments was less than optimal. This was well documented by the Campbell report, which examined the management of the outbreak in Ontario (SARS Commission 2004). The report, in particular, identified the dysfunctional relationship between the provincial chief medical officer and federal officials. The poor relationship had several consequences, including inadequate data transfer to the federal level and the recall of federal field epidemiologists from Ontario due to lack of clarity as to their role. The problems with intergovernmental cooperation were noted not only in Canada but also by international agencies. David Heymann of the WHO commented:
SARS has shown us that relationships between federal, or central, and provincial or state governments are very important in public health, and very difficult to establish…We understand that this has been a problem in China. It certainly has been a problem in Canada, where there have been difficulties between Health Canada and the provincial government. (Alphonso and York 2003, A1, A6)
Concerns over the existing emergency legislation and the limitations on federal power were highlighted in the reports by Dr. Naylor and Senator Kirby (National Advisory Committee on SARS and Public Health 2003, executive summary; Standing Senate Committee on Social Affairs, Science and Technology 2003). Advocating legislative renewal as a possible solution, the Canadian Medical Association (CMA) has proposed a Canadian Emergency Health Measures Act based on a health-alert system.6 This proposal outlines five levels of health alert. For each level it describes associated governmental powers, whether consent of the province is required for action and who the lead response team would be. For example, in a level 1 alert mandatory surveillance would be required, and the lead response team would be municipal or provincial. In a level 5 alert, powers would include regulation or prohibition of travel and evacuation of persons, and there would be an international lead response team. The CMA proposal also suggests that the share of federal funding of the crisis should progressively increase as the level of alert increases (Canadian Medical Association 2003). The Naylor report supported this approach and in particular highlighted the importance of a having a graded system, commenting:
As the level of government uniquely charged with protecting the national interest, the federal government has the strongest legitimacy to act alone when an infectious outbreak potentially has interprovincial and/or international dimensions. Moreover, it enjoys a comparative institutional advantage in regulating matters with an interprovincial or international dimension. Conversely provincial public health officials enjoy the greatest legitimacy in responding to outbreaks that are largely local in impact. A graded approach to federal intervention would complement, rather than replace, existing provincial and municipal public health structures, helping again to stitch them together into a national system. (National Advisory Committee on SARS and Public Health 2003, chap. 9, 177)
The Kirby report echoed these sentiments and endorsed a mildly modified version of the CMA system. While many of the recommendations of both the Naylor and Kirby reports have been implemented, little progress has been made in relation to their recommendations regarding the need for new emergency legislation.
Continued vulnerability to the sort of defective intergovernmental cooperation that occurred during the management of SARS clearly is not acceptable. Many of the current reform initiatives have attempted to address these dysfunctional relationships, primarily by developing better communication strategies and intergovernmental interfaces. Ottawa has moved on two broad fronts to improve its capacity on public health emergency preparedness and response. The first front is the so-called federal strategy on public health. Led by the minister of health and the recently appointed minister of state for public health, this strategy is composed of three key elements: the creation of the Public Health Agency of Canada (PHAC), the appointment of a chief public health officer for Canada and the development of the Pan-Canadian Public Health Network.
In terms of emergency response, the PHAC and the new chief medical officer are intended to “coordinate federal efforts in identifying and reducing public health risks and threats and support national readiness to respond to health crises” (Public Health Agency of Canada 2004a). They are meant to show public leadership in the event of a crisis and to work continually to improve intergovernmental collaboration in public health emergency preparedness. At the same time, the PHAC and the chief medical officer will coordinate Canada’s interaction with various international public health agencies and bodies such as the World Health Organization, the US Centers for Disease Control and Prevention and other agencies in Asia and Europe. The third element, the Pan-Canadian Public Health Network, is still very much a work-in-progress. This network is designed to build on the efforts of federal and provincial ministers of health, who in 2003 agreed to work collaboratively on a number of key issues related to emergency response (e.g., clarification of roles and responsibilities, improving the surveillance and information structure, creating a national network of public health science centres and resolving issues related to health human resources). The Pan-Canadian Public Health Network is a federal-provincial initiative, approved by the ministers of health, that subsumes and will coordinate the various mechanisms and arrangements that currently exist for intergovernmental collaboration on public health matters. While each of these elements is designed to better coordinate efforts in public health generally, they are also clearly meant to enable federal leadership in the event of another public health emergency like SARS (Public Health Agency of Canada 2004b).
The second front of the federal response is contained in the government’s new national security framework and action plan, Securing an Open Society: Canada’s National Security Policy (Privy Council Office 2004). This framework seeks to build a fully integrated security system that brings together and provides tools to better coordinate the federal government’s security capacity. In terms of emergency response, the framework calls for the creation of an integrated threat assessment centre to gather threat-related information; a government operations centre to coordinate federal efforts during emergencies; a review of the Emergency Preparedness Act; and the creation of a permanent federal-provincial-territorial “high-level” forum on emergency management. An integral part of this framework is the identification of the international migration of infectious diseases and the possibility of bioterrorist attacks as key security threats to Canadians. The national security framework intends to integrate efforts to renew the federal leadership in public health and the government’s broader action plan for emergency preparedness.
Despite the several reform initiatives, there remain shortcomings with the current set of intergovernmental arrangements, which depend upon the voluntary cooperation of provinces at the time of a public health crisis. Fundamentally the issues relate to externalities and spillovers of disease outbreaks. A disease developing in one province affects not only that one province; it has the potential to affect other provinces across the country, either directly through spread of the disease or indirectly through stigmatization of the affected region. Thus, in many respects, the management of a disease outbreak is of national concern. If a province has the resources to adequately manage the outbreak, there would be no requirement for assistance from the federal government. However, at a minimum, a province should communicate information on the outbreak openly to other governments. Such information would allow adjacent provinces to prepare for the potential spread of the disease. Nevertheless, there are real disincentives for any provincial government to provide detailed reporting of the status of an outbreak, particularly at an early stage when there is uncertainty about the outbreak’s magnitude and when such reporting could, perhaps unnecessarily, adversely affect the province’s industries and tourism. Thus, it is conceivable that a province would be reluctant to report an outbreak out of fear of negative economic consequences or simply out of a belief that the matter was within their sole jurisdiction. This would be particularly worrisome if a province proved not to be able to manage the outbreak effectively on its own and had not provided adequate reporting to other governments. Apart from the health impacts of spread of the disease across the country, there would also be concerns about the potential for stigmatization, which would likely not be confined to the province initially affected, particularly if international attention were drawn to the outbreak. Similarly, if an outbreak involved a specific industry within the affected province, and international attention were drawn to the matter, that industry could be affected nationwide. The federal government might also have a disincentive to report on the status of an outbreak, but since its electoral accountability is to the entire country, rather than only to the region where the outbreak would be occurring, the disincentive to report is comparatively less than that experienced by a single province.
A vivid illustration of the importance of a national approach to combatting a developing outbreak is provided by two simulations of a human-to-human avian flu outbreak developing in Thailand (Ferguson et al. 2005; Longini et al. 2005). While varying in their estimation of the potential severity of the outbreak, both simulations do suggest that the outbreak could be stopped with aggressive early interventions. These interventions would include pre-pandemic flu vaccination, social distancing measures such as quarantine and the targeted distribution of antiviral treatments. While an emerging human avian flu pandemic in Canada would have different characteristics, the fundamental principles of the response to the outbreak would likely apply in this country as well. Early detection of the outbreak and the mobilization of adequate public health resources to introduce preventative measures would be necessary to halt the epidemic. Such an operation would likely require a national effort with public health resources from the entire country being diverted to the affected province. Ideally this would be a collaborative enterprise between the Public Health Agency of Canada and provincial and local public officials. However, if for some of the reasons described above a province were slow to report the outbreak or hesitant to allow federal involvement, an otherwise preventable epidemic might spread to adjacent provinces. While federal intervention would by then be permissible, the window of opportunity for effective action would have passed.
The emergence of an international strategy to combat pandemic infections adds to the urgency of addressing Canadian governance strategies for the management of infectious outbreaks at a national level. A new model of global health governance has recently emerged, principally in response to SARS. A key component of this more aggressive approach to the management of pandemics concerns the responsibility of individual nations to the global community with regard to adequate national surveillance and communication of the status of outbreaks to the World Health Organization (WHO). Canada’s roles and responsibilities as part of the larger international community provide compelling reasons for a re-evaluation of the current federal approach to public health emergencies.
In many ways the international health community could be viewed historically as a confederation, with the WHO acting on behalf of member states of the World Health Assembly. In this model, the WHO was necessarily subordinate to the member nations, in accordance with the principle of the primacy of national sovereignty. As well described by David Fidler, Lawrence Gostin and others, however, there has been a transformation in this governance regime (Fidler 2003a, 2004; Gostin 2004; Kickbusch 2000). Now, in times of disease outbreaks, the WHO can act in many ways as the central authority with considerable coercive power over its member states.
As Fidler has set out, global germ governance has been transformed from a horizontal governance regime to one that is more characterized by vertical governance (Fidler 2003b). In the horizontal governance regime the objective of the International Health Regulations, the primary piece of legislation governing the international management of disease outbreaks, was to prevent the spread of disease from nation to nation with minimal interruption of international traffic or trade. In this governance regime the sovereignty of individual nations was paramount, and the WHO did not have the authority to act in a member nation without its permission. In the transition to a vertical governance regime, however, the WHO has begun to act directly within member nations to control the spread of disease. The management of SARS demonstrated how aggressive this governance regime could be, largely as a consequence of two new approaches the WHO has adopted. The WHO has received authority from the World Health Assembly to use nongovernmental sources of information to track the spread of disease (World Health Organization 2002). An application of this is the use of information provided by the Global Public Health Intelligence Network (GPHIN). GPHIN was developed by Health Canada and is employed by the WHO to scour international Web sites for evidence of disease outbreaks (Public Health Agency of Canada 2005).7 The ability to use nongovernmental sources of information is significant because it allows the WHO to conduct surveillance without member nation permission. The second component of what Fidler describes as the WHO’s “double-pincer” power over member nations is the WHO’s ability to issue travel advisories (2004). Though they were not officially authorized, travel advisories were used by the WHO in combatting SARS (World Health Organization 2005). And while there was some disagreement with the decision to issue travel advisories based on scientific grounds, the right of the WHO to issue such advisories appears not to have been questioned. The ability to conduct independent surveillance and to make unilateral declarations of travel advisories provides the WHO with considerable power to govern the international management of an outbreak. Specifically, attempts by countries to withhold information will likely ultimately fail — due to the acquisition of information from nongovernmental sources — and result in penalties in the form of travel advisories.
This changing state of international governance has important implications for Canada. Our federal government must have the ability to acquire complete knowledge of an outbreak in order to adequately meet the reporting requirements of the WHO. While this transfer of information from provincial to federal levels could occur voluntarily, the SARS outbreak demonstrated the dangers of relying upon voluntary communication. The following comments by a federal official quoted in the Campbell report illustrate this challenge:
The challenge for us, nationally, was to have as much information as possible and as much information as possible that had been analyzed by Ontario, at least initially, in order to ensure that we had as complete a picture as possible of the situation in Canada, primarily in Ontario [and] that we could then share that information with other countries and with the WHO, in order to be able to demonstrate that we were responding appropriately…I don’t think we really ever felt that we were working in true partnership with the Province [Ontario]….And that inevitably led to a sense of confusion in the outside world, WHO and other countries, as to how far we had this under control. (SARS Commission 2004, 66, 68)
Consider the possibility of a new infectious agent emerging in a Canadian province. Initial outbreak management would again be local, with supervision by the province. The revised International Health Regulations require adequate surveillance of the outbreak and communication of the status of the outbreak to WHO officials (World Health Organization 2005). There is a possibility, however, that the federal government may not be able to meet its reporting requirements because of a lack of intergovernmental cooperation within Canada. While the WHO would have mechanisms to obtain this data from nongovernmental sources, if the WHO had to resort to such measures to monitor the outbreak, its confidence in Canada’s ability to manage the outbreak would most certainly be undermined. In this eventuality, the WHO would have the authority to issue recommendations to prevent the international spread of the disease, which could include recommending restricting travel to affected parts of Canada. Of much greater concern, of course, would be a scenario where lack of intergovernmental cooperation led to suboptimal management of an outbreak that, in turn, contributed to the international spread of the outbreak. The danger posed by such a failure is particularly acute if, as a consequence, the outbreak spreads to a developing country. Given the lack of resources in developing countries for managing outbreaks, the spread of disease to one of these countries could be devastating for its population. If such an event occurred, Canada’s intergovernmental failure would be viewed as intolerable and unacceptable from the perspective of the international health community.
As we have outlined, there are compelling reasons for stronger federal authority to manage disease outbreaks. At a minimum, detailed knowledge of the outbreak is necessary at the federal level for several reasons, including the need to prepare for federal intervention in the event that the outbreak exceeds the management capacity of the province; communication with adjacent provinces so as to allow them to adequately prepare for any spread to their regions; and communication with the international community. Additional federal powers for direct action within the confines of a province may also be required to address an outbreak that is not being managed adequately and poses a threat to the country as a whole. Moreover, previous experience with SARS has demonstrated that we cannot necessarily rely upon cordial relations among the various orders of government at times of crisis. The structure of relations between federal and provincial orders of government is thus central to Canada’s capacity to manage future infectious outbreaks. In general, four options are available to federal officials in considering how to address this issue: a distentangled approach, a collaborative approach, an hierarchical approach and a confederal approach (Lazar and McIntosh 1998).
In a “disentangled” approach to emergency public health response, federal and provincial officials would work within their own constitutionally defined areas with limited interaction. There are problems with this. First, such an approach implies there are cleanly divided constitutional responsibilities. As has been clear from analyses of public health law in Canada, however, there is considerable overlap of jurisdictional responsibilities (Jackman 1996; Braen 2002). While management of an outbreak is within the jurisdiction of a province, the potential for the outbreak to involve other provinces and the country as a whole creates a constitutional basis for federal involvement.
Second, a fundamental problem that has been consistently identified in analyses of public health in Canada has been the lack of coordination of activities among all orders of government and public health partners. Previous descriptions of public health in Canada have used the term “islands of activity” in describing the lack of coordination (Wilson 2001). In doing so, these descriptions draw attention to the potential for overlap and, of more concern, gaps in critical public health functions. The disentangled approach, together with the lack of clarity on governmental roles and responsibilities, would perpetuate this situation and thus jeopardize the effectiveness of public health activities.
The post-SARS approach to public health is arguably collaborative, and there are clear reasons why governments at all levels — local, regional, provincial and federal — have chosen this path. Public health requires sharing of information and coordination of activities for many of the reasons described above. Furthermore, there are real limitations on the federal government’s ability to act in the absence of provincial and local cooperation, even in those areas in which the federal government has legislative authority. An example can be found in health protection, where the federal government is able to pass regulations requiring certain levels of safety standards. However, the capacity of the federal government to police these standards nationwide is clearly limited and must be enhanced with provincial cooperation.8 This need for cooperation is magnified in areas such as health surveillance, where the ability of the federal government to collect data on acute and chronic diseases is clearly beyond the resources available to it on the ground.
It thus makes sense to rely, at least in part, on a collaborative approach among governments in dealing with public health emergencies. The federal government cannot afford to alienate provincial and local public health officials with a heavy-handed, top-down approach when the greatest understanding of the nature of the threat is often at the local level. Furthermore, it is the local public health officials who will be the backbone of the response and have an intimate understanding of the environment in which the problem has emerged. The recent public health reform initiatives described earlier have recognized these realities and have implemented several mechanisms to enhance intergovernmental cooperation. The model for the new Public Health Agency of Canada is largely collaborative, with a primary strategy of facilitating coordination by providing seed funding to develop desired programs. An important further step would be to ensure that provincial and federal emergency legislation are complementary. To do so the federal government could create an equivalent of the US Model State Emergency Health Powers Act, for the provinces to emulate (Gostin et al. 2002).9
However, there are also risks in assuming intergovernmental relationships will work effectively in times of crisis. In the United States, one scholar has commented that at times of crisis the different orders of government are indeed able to come together to address the challenge (Parmet 2002). This was particularly evident after September 11 and the anthrax attacks. Nevertheless, despite the extensive efforts to prepare for an emergency post-September 11, Hurricane Katrina and the flood in New Orleans revealed the susceptibility of the United States to intergovernmental jurisdictional confusion during a crisis (“Katrina” 2005). Lack of coordination of the intergovernmental response has been blamed for contributing to preventable morbidity and mortality. Local and state officials have criticized the federal response for not providing assistance rapidly enough. Conversely, federal officials have stated that there was a lack of cooperation among state and local officials and that the federal government had not been officially invited in — as is required under American law — at the earliest stages (Stout 2005). In light of the inadequate handling of the Hurricane Katrina emergency, the United States is considering the option of federalizing emergency response, although this has provoked opposition from state officials (Bush 2005).
New Orleans should serve as a further warning to Canadian officials of the potential danger of relying solely upon collaborative relationships during a crisis. Regardless of which order of government had the primary responsibility to respond to the crisis and regardless of which order of government was primarily responsible for the lack of a coordinated response, to date at least, the federal government has received the majority of the blame. There appears to be an expectation that in disasters of this proportion, the responsibility to manage the crisis is primarily federal, regardless of the constitutional division of powers and existing legislation in the area. For Canada, the lesson is straightforward. The federal government must have a contingency plan in the event of shortcomings in intergovernmental relationships. It must be able to act with great speed, as infectious diseases can spread rapidly. As already stated, we believe effective intergovernmental collaboration is the best strategy for managing an infectious outbreak, and it would be optimal if these relationships were formalized through pre-existing memoranda of understanding. We also believe, however, that Ottawa should not put all its eggs in one basket. This brings us to a third governance option.
As part of a contingency plan the federal government could proceed with a more hierarchical approach through a set of policy initiatives.10 First, Ottawa could proceed with a legislative option. The federal government could amend the current emergency legislation, specifically stating that, for a public health emergency in which the properties of the crisis suggest rapid transmissibility, the federal government would have the authority to intervene without provincial permission. One criterion for invoking the legislation could simply be that the existence of the crisis in more than one country demonstrates a substantial risk of cross-border transmissibility. Alternatively Parliament could be asked to enact new and separate emergency public health legislation that would provide the requisite authority. The merits of these different approaches are discussed later in the paper.
Several options exist for the federal government to argue the constitutionality of such legislation. Historically, federal health protection legislation has been supported on the basis of the federal criminal law power permitting Ottawa to take measures to protect against an “evil” that is a danger to the public.11 The federal government could also rely upon its rarely used powers under the “peace, order and good government” (POGG) clause. In doing so it might well be able to rely upon either the national concern branch or emergency powers branch of POGG. A previous ruling has invoked pestilence as an example of where the emergencies clause of POGG could be employed.12 Perhaps more compelling is the argument in favour of using the national concern branch (Choudhry 2002). Previous rulings have suggested that this branch may be invoked when intra- and extraprovincial implications of the issues are linked, provinces are not able to regulate effectively on their own, and failure of one province to regulate would affect the health of residents of other provinces (Jackman 2000).13 Public health emergencies, particularly an infectious outbreak, could be seen to meet these criteria. Ultimately, of course, it would be up to the courts to decide on the constitutionality of any new federal legislation. We would hope that an awareness of the increased globalization of the world and the recognition of our international responsibilities would favour the courts granting the federal government the necessary powers.
A second issue would be to define what specific powers the legislation would provide the federal government. Options range from simple oversight authority, to access to all data, to the ability to assume control of institutions. The CMA model of tiered emergency public health legislation, which confers different levels of powers on the federal government depending on the nature and extent of the crisis, may be a mechanism by which to reassure provinces that the federal government would be limited in its recourse to these additional powers. We will discuss these options in further detail later in this paper.
Obviously, there are important limitations to the use of a federal legislative option that would need to be considered. Whatever powers the legislation provided the federal government, Ottawa would need to have the capacity to carry out the powers. There is a question of whether the federal government has sufficient capacity, particularly with respect to the number of trained personnel, to assume command-and-control responsibilities in the event of an outbreak. There are also limitations on the federal capacity to enforce any power it may have on matters such as surveillance, and some level of collaboration is necessary even when the federal government has legislative authority. Therefore, questions that would need to be addressed concerning a federalized emergency response include the following: What existing public health personnel would Ottawa have available to assist in managing the crisis? Would the federal government have the authority to transfer public health personnel from other regions of the country to the affected region? Under what conditions could the federal government employ the Canadian Forces to carry out functions such as enforcing quarantine and distributing therapies and prophylactic measures? How exactly would the federal government structure its relations with a provincial government to maximize cooperation, given that the majority of the personnel that the federal government would commandeer would be provincial?14 The complexity of many of these issues requires that the federal government use any powers provided by legislation in a respectful manner, so as to secure the provincial and local cooperation needed for an effective response. Respectful exercise of federal powers would, for instance, dictate that the use of federal powers be restricted to appropriate circumstances and that federal actions be intended to add value to existing provincial and local efforts as opposed to simply replacing them. Just as important, the execution of such powers by the federal government should not create an excessive administrative or financial burden on the other orders of government involved.15
There are also nonlegislative options that the federal government could consider if it chose to proceed with a hierarchical approach. These would include employing conditional funding along the lines the federal government has chosen to use in relation to health care insurance under the Canada Health Transfer. In adopting this approach, the federal government could choose to provide large block grants to provinces in exchange for their agreeing to implement certain provisions related to emergencies. These would include, most importantly, creation of surveillance infrastructure and reporting requirements for outbreaks. A provincial concern with this strategy could be that the health care funding scenario of the 1980s and 1990s would repeat itself, with the federal government providing an increasingly smaller proportion of emergency-response funding over time (Wilson 2000).
The federal government could also choose to bypass the provincial governments and interact directly with regional public health units through contracts. By doing so, it could provide seed funding to local public health units in exchange for the development of necessary programs for emergency public health response. In some ways the current model for the Public Health Agency of Canada allows for this option, although seed funding must be within the framework of an agreement with the province or territory concerned. A primary objection to this approach would be a perception that the federal government was invading provincial jurisdiction.
An intriguing alternative to federal involvement in public health emergency response is a confederal approach. This would entail provinces working together in the absence of the federal government or with the federal government as a partner, but with provincial governments having primacy (Courchene 1997). Such an approach may be reasonable on a regional basis for some public health issues in which spillovers are in adjacent regions (e.g., water, air) as opposed to those issues in which spillovers are national (e.g., disease and food safety). In many respects confederal approaches are under way through several national public health networks. An example of a successful confederal organization is Canadian Blood Services (CBS), a national (excluding Quebec) not-for-profit organization (Sher 2004). In the CBS model, the members are the provinces, who are responsible for funding the organization. CBS’s operations are at arm’s length from government, and the organization conducts its work through many regional offices. However, it is important to recognize there is a responsibility to meet federal standards in relation to blood safety under the Food and Drug Act.16 The CBS model would have to be considered a success as it has created, in the wake of Canada’s largest public health catastrophe — the transmission by transfusion of HIV and hepatitis C — an organization that has received high marks from hemophiliacs, one of the groups that were primary victims of that catastrophe (Canadian Hemophilia Society 2005). The establishment of the Pan-Canadian Public Health Network provides an example of the development of a confederal relationship among public health authorities across Canada.
How, then, should the federal government proceed in defining its relations with the provinces regarding the management of public health emergencies? Inevitably relationships must be collaborative, given the importance of coordination, the recognition that local public health officials are the first line of defence against the emergency, and the general recognition of the need to share capacity. Therefore any redefinition of a federal role must build upon and nurture existing collaborative efforts. Furthermore, the collaborative option should be the first option considered when a public health emergency presents itself. Similarly, the federal government and provinces/territories should continue to develop national public health networks, analogous to confederal relationships, which will provide on-the-ground capacity and build the effective relationships that can be called upon at a time of crisis.
Nevertheless even these two approaches together are not necessarily enough, and we believe that a federal “hierarchical” option needs to be incorporated into the current emergency-response strategy. While considerable effort has been undertaken to develop strong collaborative relationships, the experience with the SARS outbreak showed that the federal government cannot necessarily rely upon provincial goodwill in times of crisis. The current system needs to be insulated against the prospect of the missteps that occurred during the SARS outbreak being repeated.17 An additional advantage of a federal hierarchical approach is that it could further encourage collaborative approaches to be taken from the outset. If the provinces recognize that the federal government has a hierarchical alternative in the event that intergovernmental cooperation fails, they may have a greater incentive to cooperate at the early stages of an outbreak, which would clearly be preferable. Several issues need to be clearly outlined, however, if the federal government chooses to pursue a legislative option.
Assuming that a legislative strategy is to be pursued, two options are available to the federal government. A minimal measure would be to amend the existing emergency legislation to make special provisions for public health emergencies that have the potential to cross provincial borders or that have already crossed international borders. The second option would be to remove public health emergencies from the existing legislation and deal with them in separate new public health emergency legislation. This would allow the legislation to expressly include provisions to address the nuances of specific public health emergencies. While we have focused on the possibility of an infectious disease outbreak, other public health emergencies also present unique management challenges. Thus, separate public health emergency legislation would be able to be directed at the specific properties of the health emergency in question.
As now written, the Emergencies Act deals with four broad categories of situations: war emergencies, public-order emergencies, international emergencies and public welfare emergencies. The case for distinguishing public welfare emergencies, and specifically that component of public welfare emergencies that relates to public health, from the other three types is that public health emergencies present a significantly different type of situation from that of the other three.18 In the first three cases, the use or the threat of the use of violence is paramount. In contrast, a “public welfare emergency” refers to situations caused by fire, flood, drought and other natural phenomena; caused by accidents or pollution; or caused by disease in human beings, animals or plants. The extent of a public welfare emergency can of course be vast, but, at least in its origins, it is not associated with the use of violence against the state and its democratic institutions. In the first three situations, government is more likely to resort to actions that rest uneasily with basic freedoms. Proclaiming emergency authority in those situations may often provoke objections from opposition parties, human rights groups, minorities or other affected parties, so the threshold of danger might have to be very high before a federal government would be willing to use such powers.
The downside, therefore, of continuing to include public welfare emergencies, and specifically public health emergencies, in the same statute as the other types of emergencies is that the public welfare emergency may be “tainted” by its association with its potentially more draconian cousins. And this tainting may result in the threshold for proclaiming a public welfare emergency being inappropriately high. While the current Emergencies Act already distinguishes between different categories of emergency, those distinctions would be strengthened by separate legislation. Moreover, a separate statute would allow greater flexibility for tailoring federal powers and responsibilities to the nature and extent of the public health emergency as has been described in the CMA health-alert system. Separate legislation would also allow distinctions to be made among the various types of public health emergencies beyond infectious diseases. All of this could be incorporated within existing legislation, but the extensive amendments required would be quite cumbersome.
Part I of the Emergencies Act already provides extensive powers to the federal government in the event of a public welfare emergency, including an emergency related to public health. The statute itself authorizes the Governor in Council to proclaim a public welfare emergency.19 If fully used, the powers available to the federal government under the Emergencies Act are substantial.20 It is true that the Emergencies Act calls on the federal government to exercise its powers and perform its function in a way that does not unduly impair the ability of provinces to take their own measures for dealing with the emergency in the province. And it encourages Ottawa to achieve “to the extent possible, concerted actions of a province” in the exercise of its powers.21 The Emergency Preparedness Act further exhorts Ottawa to plan its affairs such that it has cooperative agreements with the provinces in place before an emergency does occur.
For the kind of public health emergency that might occur in the future, however, these powers are not sufficient. They need to be buttressed in three ways. First, as we have described, the federal government is explicitly constrained from declaring a public health emergency where the direct effects of the emergency are confined to one province unless the provincial government indicates to Ottawa that the scope of the emergency exceeds the province’s capacity to deal with it. In our view, this limitation on the federal government must be removed for the simple reason that contagious diseases do not respect borders, whether internal or external. Thus, at the outset of an outbreak that could spread rapidly, the federal government should be empowered to mobilize the country’s resources to aggressively intervene to break the spread of the disease. We also suggest that the federal government should be empowered to take action even if a disease is not present in any province, but is present in another country and poses a real and imminent threat of spreading to Canada. In such an instance Canadian public health officials should have the authority to take the necessary measures to prepare for the eventuality of the spread of disease to Canada, including the mobilization of appropriate personnel, the distribution of preventive and therapeutic medicines and the institution of appropriate surveillance measures. Again, though ideally we would expect a collaborative approach to be adopted in order to address these issues, the federal government should be empowered to act unilaterally if required.
Second, the federal government must possess the authority to demand timely information from other orders of government. The current Emergencies Act does not explicitly grant this to Ottawa. If the federal authorities can track the pattern of disease migration, they will know whether additional powers must be proclaimed and in which areas of the country they will be needed. This kind of information flow between the Ontario and federal authorities was lacking during the SARS crisis in 2003. This additional power may raise privacy issues that will have to be worked through in a manner that recognizes competing claims for the public good.
Third, as discussed earlier, the powers of the federal government in a public health emergency are only useful to the extent that they are matched by capacity “on the ground.” This means two things: it means having the necessary public health personnel, equipment, and financial and other resources to respond, and it means having the appropriate governance arrangements to activate these resources in an efficient and effective manner.22 While existing federal law gives to Ottawa the apparent authority to commandeer doctors, nurses and hospital facilities, unless there are effective protocols specifying how such arrangements are to work, Ottawa’s statutory powers may in practice have limited effects in the communities where they are intended to apply. In this regard, it may be useful to anticipate the kinds or classes of emergencies that could arise and negotiate intergovernmental agreements (federal-provincial-regional-local) that would set out how governments would interact under each kind or class of emergency.23 The agreements would specify respective areas of responsibility, with related accountabilities. A serious obstacle to successfully negotiating such agreements, however, is simply that governments might disagree about who should do what. In particular, some provinces might be unwilling to cede broad coordinating and command powers to Ottawa. They might challenge the constitutionality of a federal assertion of such powers. They might fear the fiscal consequences of Ottawa giving directions without the certainty of appropriate financial compensation. They might even judge that the federal government would mismanage the emergency. There are two incentives the federal government might use to overcome such resistance. The first is money. Ottawa should make clear that fiscal resources will be available and, at least in part, these fiscal resources should be specified “up front.” It is not unusual for money to be used to facilitate intergovernmental relations. It should be used in this case. The second incentive that the federal government might use to secure provincial cooperation is simply to make clear that it will act alone if provincial cooperation is not forthcoming. Given Ottawa’s powers to commandeer resources, the mere possibility that it would do so without the provinces at the table should serve as an incentive for them to be there. Importantly, the recognition that the federal government has assumed these emergency powers may encourage the provinces to work with the federal government to develop complementary provincial emergency legislation so that, at least legislatively, there is a coordinated and consistent approach to an outbreak.
The existing Emergencies Act allows the federal government to invoke its emergency powers when it sees fit, subject only to very modest limitations. We would strongly recommend removing the more-than-one-province requirement for unilateral federal action. A better approach would be for the decision to permit federal involvement to be guided by the fundamental properties of an infectious threat. Federal action could be justified if the following criteria were met: (1) there is clear potential for cross-border transmission; (2) the health consequences of the epidemic are potentially severe; and (3) a national approach to controlling the outbreak could be reasonably considered to be more effective than a purely local approach.
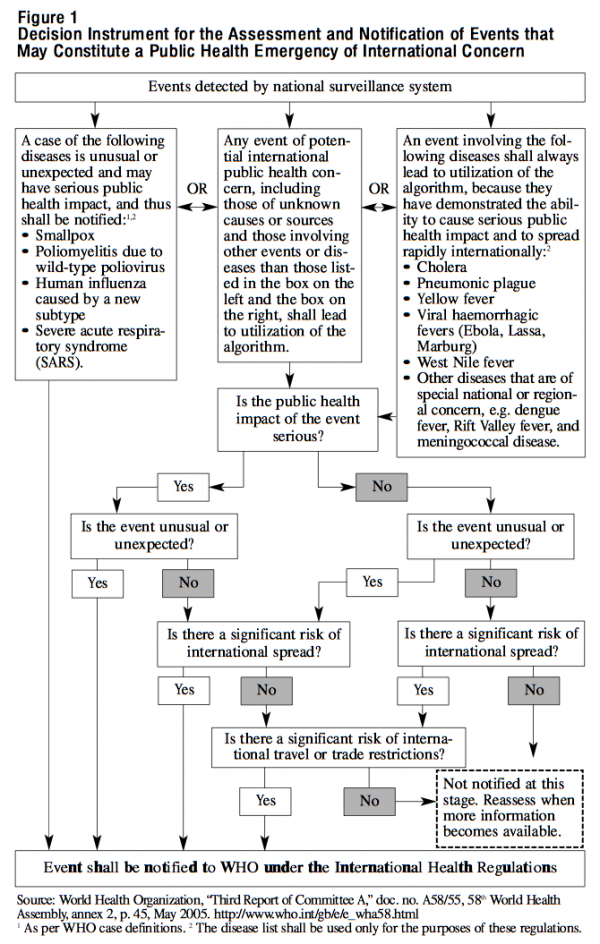
Further guidance could be dawn from the WHO’s “Decision instrument for the assessment and notification of events that may constitute a public health emergency of international concern” (see figure 1). Member nations are expected to apply this instrument to developing outbreaks within their borders. Events that constitute a public health emergency of international concern must meet at least two of the following criteria: (1) the public health impact of the event is serious; (2) the event is unusual or unexpected; (3) there is a significant risk of international spread; and (4) there is a significant risk of international travel or trade restrictions. Modifying this instrument for events of national concern and incorporating it within Canadian legislation would have two advantages. First, it would reassure provincial governments that the federal government would not use any new powers arbitrarily. Second, it would assist Canada in meeting the requirements of the revised International Health Regulations, thereby meeting our international commitments as well as potentially protecting us from WHO travel recommendations.
It was suggested above that federal money should be used to grease the wheels of intergovernmental relations. The intention here is not to anticipate the outcome of federal-provincial fiscal negotiations on cost-sharing. But it is to suggest that the wider federal powers proposed here contemplate the idea that a public health emergency in one province, or even outside of Canada, has the potential to affect the whole country. It contemplates extraordinary demands being made on, or in, one province to protect other provinces. It thus assumes that there is a national interest to be protected. Given this assumption about national interest, this suggests that the incremental cost of dealing with an emergency should be disproportionately borne by the federal authorities. And, the larger and the more costly the emergency, the greater the share that the federal government should bear. Fundamentally, it would appear appropriate to distribute the cost of responding to a public health crisis such as an epidemic, which would have the potential to cross provincial lines, across all Canadian taxpayers. Residents in Manitoba, for example, would have a clear interest in having their tax dollars devoted to controlling an outbreak in a region of Ontario that approaches their border.
In the context of the institution of a graded emergency-response system within separate public health emergency legislation, we support the CMA’s vision that the greater the level of the emergency the greater the federal responsibility for funding of the emergency response. For example, at the earliest level of an emergency, the federal government might simply require transfer of information in a timely manner and would provide funding to assist with collection of data. In the presence of a full-blown outbreak that is potentially of a national scale, the federal government might assume command-and-control responsibilities and would therefore be responsible for providing compensation to public health officials and health care workers whose services they employ. The introduction of a graded funding system to parallel the graded emergency-alert system would have the benefit of preventing the federal government from abusing its new powers since it would have to consider the potential cost of any decision to use them. In contrast, the failure to implement such a system could create unfunded mandates at the provincial level that could have serious economic consequences for the province, which may not have the resources to respond to federal demands, as well as damage future intergovernmental relationships.
Part VI of the Emergencies Act sets out the rules for parliamentary supervision of an emergency declaration. It requires the federal government to table a motion in Parliament within seven sitting days after an emergency has been proclaimed. Each house is required to debate the motion on the sitting day after the sitting day on which the motion was laid before the House and to debate it uninterrupted until it is ready for a vote. A negative vote by either house puts an end to the emergency declaration. Part VI of the Act also requires Parliament to consider a motion from either 20 MPs or 10 senators to debate a proposed revocation of all or part of the emergency declaration. There are also provisions for all orders and regulations to be laid before Parliament within two sitting days after they are made. Parliament’s existing supervisory powers seem to us to be sufficient to deal with the proposed enlarged powers that would be assigned to the federal government.
While constraints on federal authority are necessary, we nevertheless also believe that there should be a clear expectation that the federal government will use its authority when required. The federal government may be reluctant to do so because of the deterrent of assuming the cost, and responsibility, of an emergency response. To ensure that the powers are used when necessary, provinces should be able to specifically request that the federal government declare a situation a public health emergency, which would bring with it additional resources, in terms of both finances and personnel.
Ensuring that this country is prepared for the next pandemic is a high priority for public health officials. We would again like to emphasize that establishing the necessary public health infrastructure and capacity is of central importance in preparing for this threat. However, a critical component of any such preparation will be to guarantee that effective relationships exist among the various orders of government that will need to work together to manage the emergency. We have argued that an essential component of developing effective relationships is to establish a strong federal role in the emergency-response process. Strong federal leadership is essential to ensure that communication exists among provinces and with the international community. This will allow adjacent provinces and other countries to take the appropriate measures to prepare for the possible transmission of disease to their populations. It will also allow Canada to meet the requirements of the new International Health Regulations and protect itself from the avoidable introduction of travel advisories or restrictions that could have a devastating effect on regional economies.
Ideally, federal leadership would be welcomed by other orders of government and would be fully compatible with the kind of collaborative intergovernmental regime that we have previously described. At the same time, prudence requires that precautions be taken to protect against failures in intergovernmental relations. Such failures would be unacceptable to the Canadian population if they contributed to the spread of an otherwise preventable epidemic. They clearly would be unacceptable to the international community if they contributed to the international spread of disease. We have argued the best way to insulate ourselves against this occurring is to develop a federal legislative back-up plan to institute if collaborative efforts fail. This back-up plan must have necessary provisions to protect against abuse of federal powers and should be used only as a last resort if collaboration is ineffective. We believe this is best accomplished through the creation of separate federal emergency public health legislation, which could help depoliticize the declaration of a public health emergency as well as allow the legislation to be sufficiently nuanced for the particularities of different public health challenges. At a minimum we strongly recommend the removal of the “two-province clause”24 in the existing Emergencies Act, which constrains the federal government’s authority to take action. Such a provision is meaningless if the condition being addressed has the properties to rapidly cross borders or is already present in several countries.
Were the federal government to employ this legislative option, federal and provincial authorities would have to make every effort to work collaboratively to address the challenges. In addition, the federal government would have to make the necessary investments to establish the appropriate capacity to ensure it can adequately use any new powers. We would also like to emphasize that our recommendations are not meant to undermine the importance and role of local public health officials and their particular expertise but rather to protect the field of public health in general from the risk of failure of intergovernmental relations.
We believe that the issues we have described, which have also been identified in previous reports, should be addressed urgently. Global infectious health threats are increasingly being brought to our attention and at present there are international efforts to develop a coordinated approach to prepare for the next flu pandemic. In May 2005, the World Health Assembly approved newly revised International Health Regulations, which include reporting and response requirements that countries will be expected to meet within two years of the formal adoption of the regulations. The steps we have described for enhancing federal powers in the event of a public health emergency will be an important component of this country’s ability to comply with these new regulations and meet our international responsibilities — a key requirement for Canada as a member of the global public health community.
Alphonso, C., and G. York. 2003. “Canadian Health Officials Rapped by WHO.” The Globe and Mail, June 13, national edition, A1, A6.
Braen, A. 2002. “Health and the Distribution of Powers in Canada.” Discussion paper no. 2, Commission on the Future of Health Care in Canada.
Bush, Jeb. 2005. “Think Locally on Relief.” Washington Post, September 30, A19.
Canadian Hemophilia Society. Blood Safety Committee. 2005. “Report Card on Canada’s Blood System Seven Years after the Commission of Inquiry on the Blood System in Canada.” Accessed October 27, 2005. https://www.hemophilia.ca/en/10.1.4.php
Canadian Medical Association. 2003. “CMA Submission on Infrastructure and Governance of the Public Health System in Canada.” Presentation to the Senate Standing Committee on Social Affairs, Science and Technology.
Choudhry, Sujit. 2002. “Recasting Social Canada: A Reconsideration of Federal Jurisdiction over Social Policy.” University of Toronto Law Journal 52 (3): 163-252.
Courchene, T.J. 1997. “ACCESS: A Convention on the Canadian Economic and Social Systems.” In Assessing ACCESS: Towards a New Social Union: Proceedings of the Symposium on the Courchene Proposal, edited by David Cameron. Kingston, ON: Institute of Intergovernmental Relations.
Ferguson, N.M., D.A. Cummings, S. Cauchemez, C. Fraser, S. Riley, A. Meeyai, S. Iamsirithaworn, and D.S. Burke. 2005. “Strategies for Containing an Emerging Influenza Pandemic in Southeast Asia.” Nature 437 (7056): 209-14.
Fidler, D.P. 2003a. “Emerging Trends in International Law concerning Global Infectious Disease Control.” Emerging Infectious Diseases 9 (3): 285-90.
———. 2003b. “SARS: Political Pathology of the First Post-Westphalian Pathogen.” Journal of Law, Medicine and Ethics 31 (4): 485-505.
———. 2004. “Germs, Governance, and Global Public Health in the Wake of SARS.” Journal of Clinical Investigation 113 (6): 799-804.
Goel, Vivek. 2004. “What Do We Do with the SARS Reports?” Healthcare Quarterly 7 (3): 28-41.
Gostin, L. 2004. “The International Health Regulations and Beyond.” Lancet Infectious Diseases 4 (10): 606-7.
Gostin, L.O., J.W. Sapsin, S.P. Teret, S. Burris, J.S. Mair, J.G. Hodge, Jr., and J.S. Vernick. 2002. “The Model State Emergency Health Powers Act: Planning for and Response to Bioterrorism and Naturally Occurring Infectious Diseases.” Journal of the American Medical Association 288 (5): 622-8.
Hogg, Peter W. 2004. Constitutional Law of Canada, student ed. Scarborough: Thompson Canada.
Institute of Medicine. Committee for the Study of the Future of Public Health, Division of Health Care Services. 1988. The Future of Public Health. Washington, DC: National Academy Press.
Jackman, M. 1996. “The Constitutional Basis for Federal Regulation of Health.” Health Law Review 5 (2): 3-10.
———. 2000. “Constitutional Jurisdiction over Health in Canada.” Health Law Journal 8: 96.
“Katrina Reveals Fatal Weaknesses in US Public Health.” 2005. Editorial, Lancet 366 (9489): 867.
Kickbusch, I. 2000. “The Development of International Health Policies — Accountability Intact?” Social Science and Medicine 51 (6): 979-89.
Lazar, H., and T. MacIntosh. 1998. Federalism, Democracy and Social Policy: Towards a Sectoral Approach to the Social Union. Kingston: Institute of Intergovernmental Relations, Queen’s University.
Longini, I.M., Jr., A. Nizam, S. Xu, K. Ungchusak, W. Hanshaoworakul, D.A. Cummings, and M.E. Halloran. 2005. “Containing Pandemic Influenza at the Source.” Science 309 (5737): 1083-7.
Mackay, Brad. 2003. “Toronto Quarantines Patients as SARS Concern Grows.” e-CMAJ, March 26. Accessed October 31, 2005. https://www.cmaj.ca/news/ 26_03_03.shtml
National Advisory Committee on SARS and Public Health. Dr. David Naylor, chair. 2003. Learning from SARS: Renewal of Public Health in Canada. Ottawa: Health Canada.
Parmet, W.E. 2002. “After September 11: Rethinking Public Health Federalism.” Journal of Law, Medicine and Ethics 30 (2): 201-11.
Privy Council Office. 2004. Securing an Open Society: Canada’s National Security Policy. Ottawa: Privy Council Office.
Public Health Agency of Canada. 2004a. “The Public Health Agency of Canda.” Information Backgrounder, September. Accessed November 1, 2005. www.phac-aspc.gc.ca/media/nr-rp/2004/phac_e.html
———.2004b. “Public Health in Canada.” Presented to the Public Health Education Project: Pudong, New Area of Shanghai, Centre for Wellness Research and Education,York University. Accessed November 1, 2005. www.yorku.ca/wellness/shanghaihealth/phac.ppt
———.2005. “The Global Public Health Intelligence Network (GPHIN)” Accessed October 21, 2005. https://www. phac-aspc.gc.ca/media/nr-rp/2004/2004_ gphin-rmispbk_e.html.
SARS Commission (Commission to Investigate the Introduction and Spread of SARS in Ontario, the Hon. Archie Campbell, commissioner). 2004. The SARS Commission Interim Report: SARS and Public Health in Ontario. Toronto: Government of Ontario.
Sher, G.D. 2004. “The Blood Supply System in Canada.” Presented to Advisory Committee on Blood Safety and Availability. Ottawa: Blood Services Canada. Accessed October 24, 2005. https://www.hhs.gov/bloodsafety/presentations/BloodSupplySystemIn Canada.pdf
Standing Senate Committee on Social Affairs, Science and Technology. Michael Kirby, chair. 2003. Reforming Health Protection and Promotion in Canada: Time to Act. Ottawa. Accessed October 24, 2005. https://www.parl.gc.ca/37/2/parlbus/commbus/senate/com-e/soci-e/rep-e/repfinnov03-e.pdf
Stout, D. 2005. “Former FEMA Chief Blames Local Officials for Failures.” New York Times, September 27.
Svoboda, T., B. Henry, L. Shulman, E. Kennedy, E. Rea, W. Ng, T. Wallington, B. Yaffe, E. Gournis, E. Vicencio, S. Basrur, and R.H. Glazier. 2004. “Public Health Measures to Control the Spread of the Severe Acute Respiratory Syndrome during the Outbreak in Toronto.” New England Journal of Medicine 350 (23): 2352-61.
Wenzel, R.P., and M.B. Edmond. 2003. “Managing SARS amidst Uncertainty.” New England Journal of Medicine 348 (20): 1947-8.
Wilson, K. 2000. “Health Care, Federalism and the New Social Union.” Canadian Medical Association Journal 162 (8): 1171-4.
———.2001. “The Role of Federalism in Health Surveillance: A Case Study of the National Health Surveillance ‘Infostructure.’” In Federalism, Democracy, and Health Policy in Canada, edited by D. Adams. Kingston: McGill-Queen’s University Press.
———.2004. “A Canadian Agency for Public Health: Could It Work?” Canadian Medical Association Journal 170 (2): 222-3.
Wilson, K., and C. MacLennan. Forthcoming. “Federalism and Public Health Law in Canada: Opportunities and Unanswered Questions.” Health Law Review.
World Health Organization. 2002. Global Crises, Global Solutions: Managing Public Health Emergencies of International Concern through the Revised International Health Regulations. Geneva: World Health Organization.
———.Epidemic and Pandemic Alert Response. 2003a. “Severe Acute Respiratory Syndrome (SARS): Status of the Outbreak and Lessons for the Immediate Future.” May 20. Accessed October 27, 2005. https://www.who.int/csr/sars/resources/ en/index.html
———.2003b. “WHO Extends Its SARS Related Travel Advice to Beijing and Shanxi Province in China and to Toronto Canada.” Notes for the Media, April 23. Accessed October 24, 2005. https://www.who.int/mediacentre/ news/notes/2003/np7/en/
2005. “Third Report of Committee A.” Doc. no. A58/55, 58th World Health Assembly, May. Accessed November 3, 2005. https://www.who.int/gb/e/e_ wha58.html
This publication was produced under the direction of France St-Hilaire, Vice-President, Research, IRPP. The manuscript was copy edited by Tim Niedermann, proofreading was by Riça Night, production was by Chantal Létourneau and printing was by Impressions Graphiques.
Copyright belongs to IRPP. To order or request permission to reprint, contact:
IRPP
1470 Peel Street, Suite 200
Montreal, Quebec H3A 1T1
Telephone: 514-985-2461
Fax: 514-985-2559
E-mail: irpp@nullirpp.org
irpp.org
All IRPP Policy Matters and IRPP Choices are available at www.irpp.org
To cite this paper:
Wilson, Kumanan, and Harvey Lazar. 2005. “Planning for the Next Pandemic Threat: Defining the Federal Role in Public Health Emergencies.” IRPP Policy Matters 6 (5).
Harvey Lazar was educated at McGill University (B.Sc.), the University of British Columbia (MA) and the London School of Economics and Political Science (Ph.D.). He served as director of the Institute of Intergovernmental Relations from 1997 to 2005. He is currently a fellow of the Institute and senior research associate at the Centre for Global Studies at the University of Victoria. He had a long career in the Canadian public service, including assignments as deputy chairman of the Economic Council of Canada (1986-92), and senior assistant deputy minister of strategic policy at Human Resources Development Canada (1992-95). Dr. Lazar contributed to a number of major research reports during his years in public service, on such diverse topics as retirement income policy, social policy, labour market development, financial institutions and foreign investment policy. His current work focuses on the Canadian social union, health governance, fiscal federalism, Canadian and comparative federalism, and the changing nature of the social contract in Western democracies in the face of globalization.
Dr. Kumanan Wilson is a specialist in general internal medicine at the Toronto General Hospital. He is an associate professor in the Department of Medicine and the Department of Health Policy, Management and Evaluation at the University of Toronto. He is also a research associate at the Institute of Intergovernmental Relations, Queen’s University, and a member of the Joint Centre for Bioethics, University of Toronto. As a Canadian Institutes of Health Research (CIHR) New Investigator, Dr. Wilson has focused on studying policy-making in areas of health protection. His work has included analyses of decision-making in the Canadian blood system and an examination of Canadian immunization policy. Dr. Wilson has also conducted research into the impact of intergovernmental relations on health policy, and he is currently examining the impact of federalism on public health. He received his MD from the University of Western Ontario and completed his fellowship training in general internal medicine at McMaster University, from where he also received his M.Sc. in health research methods.