
As the Canadian population ages, all provinces will need to expand their residential long-term care capacity to accommodate frail seniors – those who are no longer able to function independently. Conservative projections based on current trends suggest that by 2041 Canada will need 320,000 beds across the country, up from the current 200,000.
While these services are for the most part publicly funded, they are delivered by a mix of public, nonprofit and for-profit facilities. This study examines whether the type of ownership matters for the quality of care delivered.
The authors review Canadian and US research evidence on the quality of care by ownership characteristics, and consider the policy implications of this evidence. They discuss the methodological challenges associated with measuring the quality of care, and examine whether the existing research is sufficiently robust to allow us to draw conclusions on this question.
Their main conclusion is that that for-profit facilities are likely to produce inferior outcomes. While the causal link between for-profit ownership and inferior quality of care does not imply that all for-profit facilities provide poor care, the evidence suggests that, as a group, such facilities are less likely to provide good care than nonprofit or public facilities.
Yet policies in many provinces over the last decade appear to run counter to these findings, with the role played by the private, for-profit sector increasing. To reverse this trend, the authors recommend that public sector funding, rather than private capital, be used to build new facilities, and that nonprofit organizations be offered the loans and the technical support necessary to enable them to bid competitively on new residential care projects.
As the study points out, one of the principal mechanisms for generating profit is reducing staffing levels, which results in inferior quality of care. Accordingly, the authors recommend that legislated minimum staffing levels be adopted, and that adequate ongoing funding be provided to meet these benchmarks, including a budget envelope specifically dedicated to direct nursing care.
They also recommend that the following measures be taken:
Canada’s population, like those of other countries of the Organisation for Economic Cooperation and Development (OECD), is getting older. It is predicted that by 2041, 4 percent of Canadians – 1.6 million individuals – will be aged 85 and older (Health Canada 2002). Although today’s elders are living longer and are less disabled than previous generations, we can still expect the need for services to support elders who are physically and cognitively impaired to grow. These services range from light assistance with shopping, cleaning and housekeeping to more personal services, like assistance with bathing and dressing in the home setting. There will also be a need for more assisted-living facilities capable of providing additional support, such as medication administration or access to 24-hour assistance in case of an emergency, and for the most disabled elders – those who are no longer able to function independently – full facility-based long-term care with 24-hour nursing supervision.
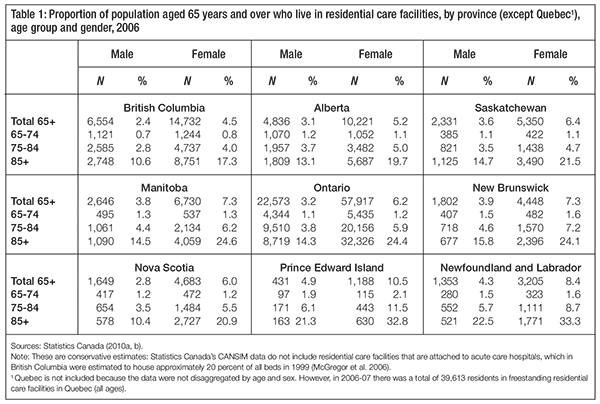
A relatively small proportion of elders currently requires residential care: one in five individuals aged 85 years and older (see table 1). Although making projections as to future needs based on current rates may be somewhat inaccurate, we estimate that by 2041, 120,000 beds will be needed in addition to the current 200,000 beds across the country (Statistics Canada 2008).1 In the years to come, therefore, all provinces will likely need to expand their residential care capacity.
Many facility residents have dementia, and the majority are women with low incomes (Cohen et al. 2005). This population is therefore highly vulnerable and has relatively little voice. Decision-makers (Medicare 2010; Ontario MOHLTC 2009; Sharkey 2008), members of the public (CBC News 2009) and academics (Harrington 2001; Kerrison and Pollock 2001) have all expressed concerns about the quality of care in residential care facilities. A number of high-profile reports addressing the quality of care (CHA 2009; CUPE 2009; Sharkey 2008), residents’ rights and public oversight of residential care (K. Carter 2009) have been published in the last two years, reflecting Canadians’ concern for the well-being of this frail population.
In many Canadian provinces, the frailty and medical complexity of facility residents are very different from what they were a decade ago. Facility residents are admitted when they are closer to the end of life. British Columbia, for example, has seen a rise in its annual mortality rates in free-standing facilities (not attached to a hospital) from 11 percent in 1997 to 17 percent in 2007 (McGregor et al. 2010b). Facility residents are also becoming more functionally dependent and require greater supervision and assistance with activities of daily living (Frohlich, De Coster, and Dik 2006; McGregor et al. 2010b).
The Canada Health Act guarantees public funding for all medically necessary services in acute care hospitals. For this reason, hospital care in Canada has remained in the quasi-public domain: hospitals are directly owned or operated by health regions, governments or largescale nonprofit societies. Unlike hospital care, long-term care is not included under the Canada Health Act. As a result, there is no uniformity of access to a defined set of services. In most provinces, long-term care is publicly subsidized; however, there is also an income-tested user-pay funding component for both home-based and residential long-term care. Furthermore, while the majority of funding remains public, service delivery is provided by a mix of public (government-owned), nonprofit and private for-profit organizations.
There has been a growing trend in some provinces to contract residential care to privately owned for-profit facilities. In British Columbia since 2000 there has been an increase of over 20 percent in publicly funded for-profit beds and a decrease of 11 percent in publicly funded nonprofit beds. In Alberta there was a 6 percent increase in for-profit beds between 2000 and 2007 (Statistics Canada 2008b, Staples and Wodok 2008), and in Ontario, almost two-thirds of new residential care beds since 1998 have been in for-profit facilities (CUPE 2009). In Quebec, the government has cut 7,632 public beds and is also expanding its funding of residential care beds in the for-profit sector (CUPE 2009; Quebec 2009).
These changes in residential care facility ownership are occurring across Canada as governments are faced with rising health system costs. The goal of this study is to review the research evidence on the relationship between types of facility ownership and the quality of residential care for frail elders, and to consider the policy implications of this evidence.
We begin with a review of the terminology and definitions and offer a theoretical overview. We next briefly describe how residential facility care fits into the rest of our health care system. This includes a discussion of what we spend on this type of care, how Canada is situated in this regard in relation to other countries, and how this varies across provinces; a breakdown of Canada’s public and private expenditures by sources and a look at how this is changing over time; and, finally, a description of the cross-Canada variation in publicly funded, private, forprofit delivery models for residential long-term care for seniors. We then discuss the challenges in conducting research that attempts to measure residential care quality.
In the next section we review the US and Canadian research evidence comparing service quality in residential care by facility ownership characteristics, the main focus of the study. This includes a discussion of whether the existing research is sufficiently robust to allow us to draw conclusions about residential care quality and facility ownership.
In the final section of the study we briefly discuss Canada’s current policy direction on this issue and propose some policy responses in light of the research evidence.
Different jurisdictions use different terminology for the institutions or homes to which disabled seniors relocate when they are no longer able to care for themselves (Hollander and Walker 2010). “Residential care for the aged” is the term used by Statistics Canada to describe institutions providing this type of care. The US describes these facilities as “nursing homes,” with subcategories for short-stay (postacute and rehab funded by Medicare) and long-stay (funded by Medicaid) beds. In Canada, Manitoba refers to “personal care homes,” Ontario has “long-term care facilities,” Saskatchewan has “special care homes,” and Prince Edward Island has “manors.”
For the purposes of this study, the term “residential care facility” refers to a facility that accommodates mainly frail older people who are unable to live independently in the community due to medical and functional frailty, and who require support and assistance with activities of daily living and 24-hour nursing supervision. This definition does not include the spectrum of seniors’ housing options that have emerged to provide living arrangements between residential long-term care and independent community living.
There is often confusion about what is meant by public, private, for-profit and nonprofit ownership. For the purposes of this study, we use the following definitions. “Public ownership” refers to facilities owned by government or quasi-governmental bodies. Municipal-care homes in Ontario, and residential care facilities owned and operated by health regions in British Columbia are examples of publicly owned institutions that provide residential long-term care for elders.
Many provinces also have long-term residential care beds and facilities that are attached to acute care hospitals. These facilities, although legally independent from government, are almost entirely government funded. Because of the amount of public funding they receive and their budgetary and organizational linkages to acute care hospitals, we consider them to be publicly owned for the purposes of this study.
There are two other main groups that provide residential care to elders. The first and largest group consists of facilities owned and operated by nongovernmental organizations. These are often religious or community groups or agencies, and the facilities they operate are run as nonprofit societies. A nonprofit society or entity is constituted with the assumption that any revenue in excess of expenses will be used to benefit its clients. Residential care facilities owned by religious or community groups (that is, not owned or operated by government or quasi-government bodies) will henceforth be referred to as “nonprofit facilities.”
The second group is made up of facilities owned and operated as businesses. Here it is assumed that revenue in excess of expenses can be directed to the owners – or, in the case of shareholder-owned companies, to shareholders. Although these for-profit facilities are often referred to as “private,” technically nonprofit facilities are also private, in that their budgets and governance are not part of a government structure. In recognition of the common understanding of “private,” we will simply refer to the former group as “for-profit” facilities. They include both small provider-owned facilities and large corporate chains whose headquarters are not necessarily in the province, or even the country, where they operate. The distinction between provider ownership and corporate ownership can be important (Harrington et al. 2001). When facility owners are also care providers, it is fair to expect that – at least theoretically – their professional obligation balances the sometimes conflicting motivations of generating profit and providing good-quality care.
A further distinction that needs to be made is that between funding and delivery of services. “Funding” relates to who pays for a service. In the case of public funding, the government pays, usually through tax revenues. In the case of private funding, the individual pays, either directly, through out-of-pocket fees, or through private insurance. “Delivery” relates to who delivers the service. The Canada Health Act effectively prohibits for-profit funding, and acute hospital care is therefore almost completely publicly funded and delivered. Residential care is not, however, covered by the Act. Therefore, there is a much greater mix of public and private, for-profit and nonprofit funding and delivery among residential care facilities. Moreover, facilities are regulated by provincial legislation, which differs among provinces.
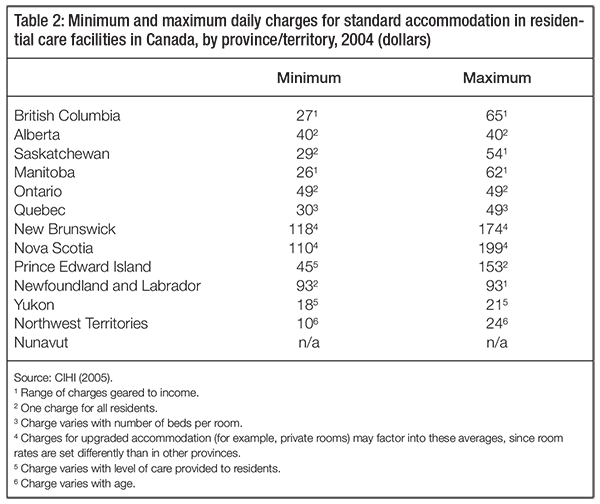
On the funding side, in residential care (unlike acute hospital care, for which user fees are prohibited under the Canada Health Act), all provinces expect residents to pay some of their accommodation fees. As summarized in table 2, these copayments are usually income tested; in 2004, maximum daily charges ranged from $21 a day in the Yukon to $199 in Nova Scotia (CIHI 2005). Also, some people have entirely self-funded private care. There are very few publicly available data for this group, which accounts for a small minority of residential care beds across Canada.
On the delivery side, although the majority of residential care facilities are publicly funded, care is provided by a mix of for-profit, nonprofit and public facilities. In publicly funded facilities the majority of beds are in the nonprofit or public sectors, except in Ontario. However, in many provinces, publicly funded beds operated by for-profit facilities are a significant and growing proportion of the total.
To complicate the spectrum of funding, delivery and ownership models even further, there has been a recent trend to diversify revenue sources within facilities. For example, in British Columbia, some nonprofit facilities have opened private user-pay wings, where those who can afford to pay receive privately financed care; and some provinces purchase services in selffunded for-profit facilities to provide certain clients with publicly subsidized residential care.
Before we proceed to our review of the research evidence and our discussion of policy, we first look at the way Canada directs resources to residential care and how it compares with other countries in this regard.
Residential care is part of a continuum of services for the aging population with disabilities. Countries and jurisdictions vary widely in their relative spending on facility-based care, assisted living and home-based care. Assisted living is considered a middle option between regulated residential long-term care and home-based care. Residential long-term care facilities are highly regulated and provide a wide range of services to significantly disabled individuals. Assisted-living facilities are less regulated and provide a limited number of support services to less-disabled seniors (McGrail et al. forthcoming). Home-based care provides services to seniors in their own homes. Home-based services include personal care (such as assistance with bathing and grooming) as well as physiotherapy and occupational therapy (McGrail et al. 2008).
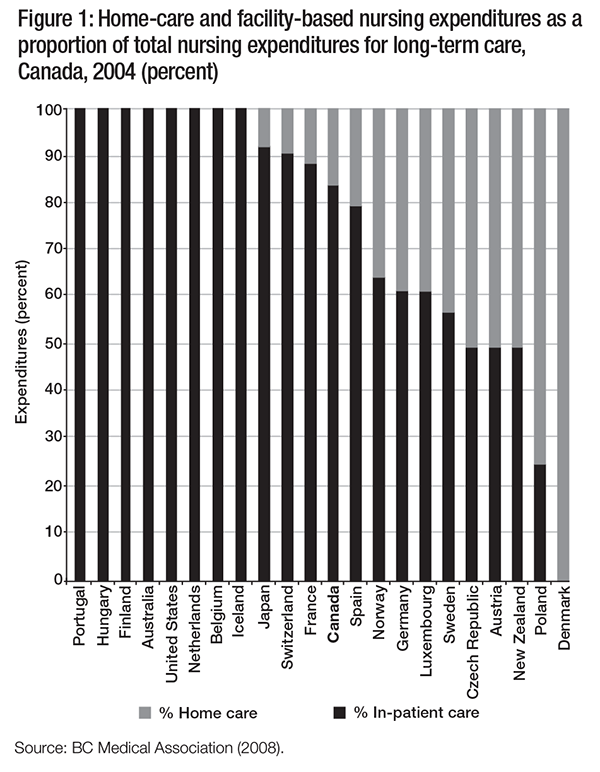
Figure 1 shows the funding that various OECD countries devote to facility-based care as a percentage of their total long-term nursing care expenditures. Almost 85 percent of Canada’s nursing expenditures in long-term care are in residential facilities; the remainder are in home care. This is somewhat more than the OECD average of 75 percent. However, in some OECD countries, such as Austria and New Zealand, nursing expenditures in long-term care are split equally between residential and home-based care (BCMA 2008).
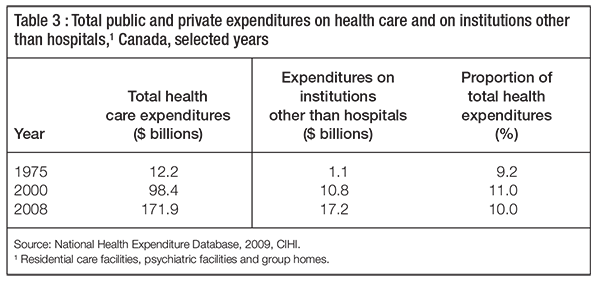
Although Canada spends slightly more than the OECD average on residential compared with home-based long-term nursing care, we spend a relatively small amount on residential care compared with what we spend on hospitals, physicians and drugs. In 2008, Canada spent an estimated $171.9 billion on public and private health care combined. The largest slice of the health care pie ($48.1 billion, or 29 percent) went to acute care hospitals. The secondand third-largest expenditure items were drugs ($29.8 billion, or 17 percent) and physicians ($23 billion, or 13 percent). Spending on residential care facilities for the elderly is included as part of “other institutions,” along with psychiatric facilities and group homes. This category was ranked fifth after other (nonphysician) professionals and is a relatively small portion – $17 billion, or 10 percent – of total public and private health expenditures (CIHI 2009).
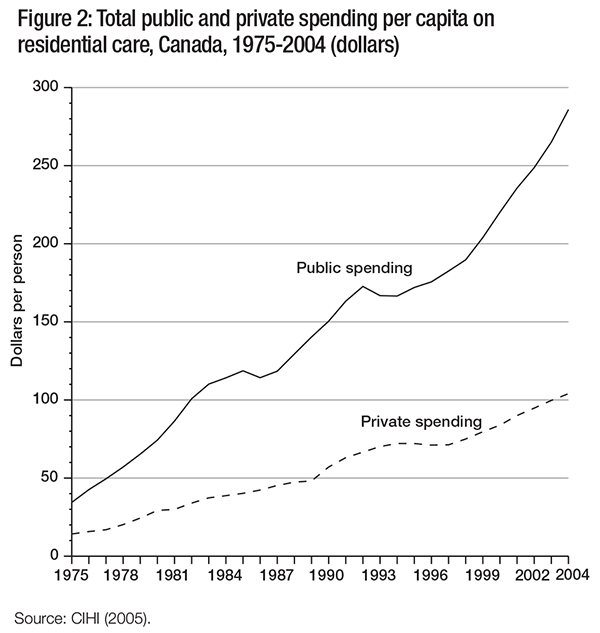
While the number of Canadians over the age of 85 has increased since 1975 and total health care expenditures have also increased, annual spending on residential care as a proportion of annual total spending on public and private health care has remained relatively constant (table 3). The amount spent per person has increased over time, however, and the rate of increase in public spending has been greater than that in private spending. Both of these points are illustrated in figure 2.
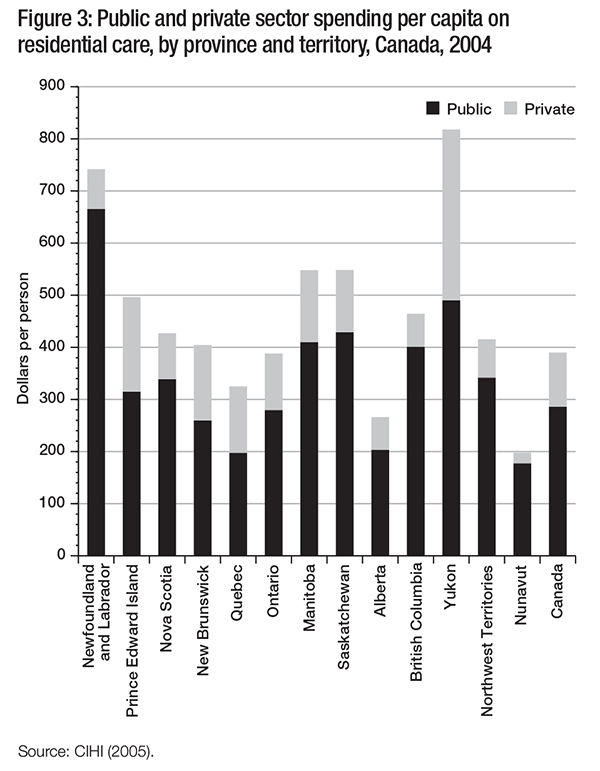
Figure 3 shows the distribution of public and private expenditures on residential care per person by province and territory in 2004. Public expenditures on residential care ranged from $178 per person in Nunavut to over $665 in Newfoundland and Labrador, while private expenditures ranged from just over $20 in Nunavut to $328 in Yukon. According to the Canadian Institute for Health Information (CIHI), these differences in spending “may reflect variations in the age distribution coverage or coinsurance across the provinces and territories” (CIHI 2005, 94). While there is substantial variation across Canada in private expenditures, these represent a relatively small proportion of total expenditures in most provinces and territories. This probably illustrates the limitations of private markets for this service – those who require residential care are often living on fixed and low incomes and cannot afford to pay privately for residential care (Cohen, Tate, and Baumbusch 2009).2
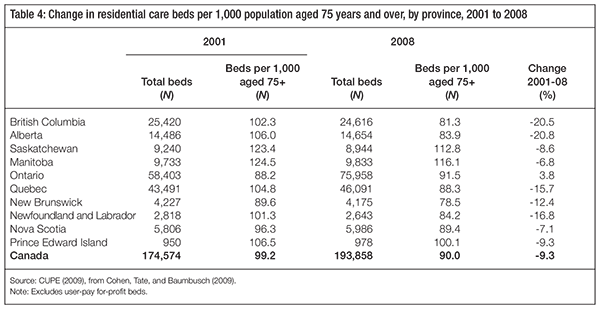
There is also great variation in the numbers of residential care beds per population of seniors across provinces (table 4). For example, in 2008, British Columbia had a residential care bed rate of 81.3 per 1,000 individuals aged 75 and older. In contrast, Saskatchewan had a bed rate of 112.8, and the national average was 90. Moreover, the trend in most provinces seems to be a reduction in the number of beds per population over time, with only Ontario showing an increase between 2001 and 2008.
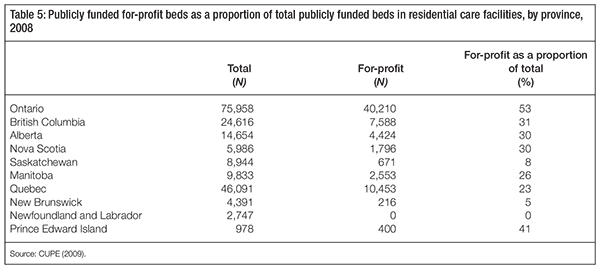
There is also considerable variation in the ownership mix of residential care facilities across Canada, which ranges from a majority of publicly funded beds owned and operated by for-profit facilities in Ontario to all publicly funded beds owned and operated by nonprofit facilities in Newfoundland and Labrador (table 5).
Table 6 describes changes in ownership status over time in British Columbia, where virtually all new publicly funded beds since 2000 are in for-profit facilities. During the same period, there have also been bed closures in nonprofit and public (health authority and hospital-based) facilities (Cohen, Tate, and Baumbusch 2009).
In Alberta, the proportion of for-profit beds in relation to the total number of publicly funded beds has increased by 6 percentage points since 2000 (Statistics Canada 2008b; Staples and Wodok 2008). In Quebec, following the release of the Castonguay report, which called for an expansion of the private sector’s role in health care delivery (Castonguay, Marcotte, and Venne 2008), the government undertook to create new long-term care beds through publicprivate partnerships (Quebec 2009). In Ontario, almost two-thirds of new beds opened since 1998 are in for-profit facilities (CUPE 2009). There is also a growing trend for larger for-profit chains to acquire smaller for-profit facilities (CHA 2009; Stocks-Rankin 2008).

Considering this mix of ownership and delivery models, our decision-makers must ensure that the funding provided to the three types of facilities, given similar residents, purchases a similar quality of care.
As is the case in other health care settings, measurement of quality in residential care facilities is not a simple exercise; the concept of quality in residential care is itself not straightforward. The American Medical Association defines quality care as “care that consistently contributes to the improvement or maintenance of quality and/or duration of life” (American Medical Association 1986). But there is no gold standard for measuring it; some have argued that the standard of quality should be facility residents’ or surrogate decision-makers’ perceived quality of life (R.A. Kane et al. 2003; R.L. Kane et al. 1983), and that this is the only measure that truly matters.
But the research on resident-centred measurement of quality is in its beginning stages, and so far most researchers have relied rather on surrogate markers they believe reflect various aspects of a facility’s quality. Much of the research by North American researchers has drawn on the Donabedian framework, which examines residential care quality in three areas: structure, process and outcome (Donabedian 1966).
Structural measures describe the physical and organizational characteristics of facilities, such as size and staffing levels (Harrington et al. 2003; Mukamel and Spector 2003). One of the most common structural measures of care quality is staffing levels. Higher nurse staffing levels have consistently been found to be associated with improved care and better outcomes (Harrington et al. 2000b). Other structural measures include turnover, training, mix and work organization of the staff; level of administrative support; building structure; and access to physicians and other paramedical support.
Process measures address the frequency of care-related activities. Studies have examined the frequency of toileting (Schnelle et al. 1988; Schnelle et al. 2001; Schnelle et al. 2004) and turning bedridden residents (Bates-Jensen et al. 2004), and the length of time spent assisting residents with feeding (Kayser-Jones 1997) as examples of care practices; greater frequency of these tasks is considered a surrogate measure of better quality (Kayser-Jones 1997). Process measures also examine the frequency of poor care practices, such as the use of physical restraints (Aaronson, Zin and Rosko 1994; Castle and Fogel 1998) and the prescription of psychoactive medications in the absence of a clear indication for such use (Hughes, Lapane, and Mor 2000). Greater frequency of these practices is a surrogate measure of poor quality.
Outcome measures in the residential care setting include the prevalence and incidence of pressure ulcers and unexplained weight loss (Arling et al. 2007; Horn et al. 2005). The rate of hospitalization for diagnoses thought to reflect care quality (care sensitive) is another outcome measure used by researchers (Ackermann and Kemle 1998; M. Carter 2003; McGregor et al. 2006; Thompson, Hall and Szpiech 1999; Zimmer and Hall 1997), although care-sensitive diagnoses have been variably defined by clinicians (Shapiro and Tate 1995) and health services researchers, adapting measures from ambulatory care settings (M. Carter 2003). Complaints (Allen, Klein, and Gruman 2003; Grabowski 2005; Stevenson 2005) and inspection violations are also considered to reflect care quality (Harrington et al. 2003; Harrington et al. 2008). Mortality is generally not considered an appropriate outcome measure, because many facility residents are approaching the end of life. However, the quality of end-of-life care is highly relevant to this population, and some authors have called for the provision of palliative care to be included as a routine measure of quality (Engle 1998).
In spite of this robust framework for considering quality measurement, researchers face a number of methodological challenges in measuring quality and in comparing quality measures between and within facilities.
One challenge is the need to rely on observational study designs to measure quality and to identify associated factors; such study designs can be more prone to biases and confounding than experimental study designs, and potentially lead to spurious correlations and the underor overestimation of effects (Gordis 2009; Rothman, Greenland, and Lash 2008). For example, the Women’s Health Initiative study discovered that prescribing hormones to postmenopausal women did not prevent them from having heart attacks; in fact, the opposite was true: women on such treatment had a higher risk of heart attack and stroke (Rossouw et al. 2002). This study discovery came after the medical community had for many years recommended hormonal treatment, based on evidence from observational studies (Anderson et al. 2004a; Lawlor, Davey, and Ebrahim 2004).
Many of the methodological challenges in observational studies that attempt to measure quality in residential care have been well described in the research literature (Mor et al. 2003). Some of the problems encountered when measuring quality in residential care are presented below.
In many cases, the outcomes we are measuring are rare events. For example, pressure ulcers (Mor et al. 2003) and formal consumer/patient complaints (Stevenson 2006) are relatively rare. As well, the denominator on which such observations is based is often small, as there are many nursing homes with fewer than 70 beds. Results based on these types of data can have statistically large standard errors and wide confidence intervals, resulting in large variations in estimates of these measures from one location and time period to the next (Mor et al. 2003).
When measuring the frequency of events such as pressure ulcers, it is important to be able to adjust for the case mix: that is, the fact that different facilities house different types of residents (Mor et al. 2003). For example, if facility X has very few mobile residents compared with facility Y, where nearly all residents are mobile, the frequency of pressure ulcers is likely to be higher in the former and the frequency of falls is likely to be higher in the latter, simply due to differences between their residents and not necessarily to the quality of care.
While quality measures address many dimensions of care, there is not necessarily a consistent correlation between one measure of care quality and another. For example, a study of nursing homes in five US states found a very low correlation between inappropriate prescribing of antipsychotics and physical restraint use (Mor et al. 2003).
Selection bias is a general term for possible bias in epidemiologic studies when the study population does not represent the target population (Delgado-Rodriguez and Llorca 2004). In this context, selection bias may be present if a facility admits a disproportionate number of a certain type of resident due to some attribute of the facility. For example, if a facility has more overhead lifts, it may end up housing a greater proportion of residents who are unable to transfer independently. If this is not accounted for, the facility may have a higher-than-usual rate of pressure ulcers because its residents are less mobile.
Detection bias is another type of potential bias in epidemiologic studies (Delgado-Rodriguez and Llorca 2004). In the context of quality measurement in residential care, an example of detection bias is when facilities with nursing staff who have the clinical acumen to detect residents’ pain report more residents being in pain than facilities where these conditions are present but go undetected and therefore untreated; the former facilities would be penalized for their nurses’ greater clinical acumen.
Censoring bias is a third type of possible bias. It occurs, for example, when a facility transfers a resident to hospital without reporting a pressure ulcer and thereby escapes responsibility for it (Mor et al. 2003). Conversely, if a resident develops a pressure ulcer while in hospital before being discharged to a facility, then the facility would inappropriately take the blame.
A further challenge in measuring quality in residential long-term care is the fact that most of the research on quality in this sector has relied on secondary administrative data; typically these data are retrospective and gathered for a purpose other than the measurement of quality per se. One example of a common secondary data source used by US researchers to measure quality is the Online Survey, Certification and Reporting (OSCAR) database (Hughes, Lapane, and Mor 2000; Konetzka et al. 2004; O’Neill et al. 2003; Stevenson 2006). OSCAR is used to access facility-level information on all US Medicareand Medicaid-funded residential care facilities, mainly for the purpose of monitoring funding.
The Resident Assessment Instrument-Minimum Data Set (RAI-MDS) is another electronic data source used by researchers to measure quality (Bates-Jensen et al. 2004; Hirdes et al. 2004; Intrator, Castle, and Mor 1999; Schnelle et al. 2003). The RAI-MDS is a screening, clinical and functional data collection system for nursing staff to assess and monitor the needs of residents; it is now widely used in residential and community care in a growing number of Canadian provinces (Broemeling et al. 2010). These data have theoretically been tested for validity and reliability. However, the RAI-MDS data were assessed in the US by the Office of the Auditor, which looked at how facility assessors evaluated the residents and entered the data used to define the residents’ level of frailty and disability. Disagreement was found between audit and facility assessors in more than 17 percent of these data elements (Mor et al. 2003). Researchers aiming to measure quality often end up deploying both OSCAR and RAI-MDS, although the variables and measures are not necessarily the most precise or appropriate.
In addition to this drawback, those collecting and entering secondary data are often busy administrators (in the case of OSCAR) or clinicians (in the case of RAI-MDS) and not researchers dedicated to measurement precision and accuracy. There is therefore often variation in the data entered, and some research has demonstrated a wide discrepancy between information recorded by staff and by residents. Schnelle and colleagues, for example, attempted to determine whether facilities’ scores for incontinence care using the RAI-MDS quality indicator correlated with facility residents’ experience of it. They interviewed incontinent residents who were capable of accurately reporting their toileting frequency. The authors concluded that the RAI-MDS incontinence care quality indicators were not related to clinically important differences in incontinence care. They further concluded that chart documentation indicating that a resident was on a scheduled toileting program or receiving toileting assistance was not related to residents’ reports of the frequency with which they received assistance (Schnelle et al. 2003).
Other secondary sources used in Canada include data on hospital and physician visits (Doupe et al. 2006; McGregor et al. 2006) and secondary survey data (Berta, Laporte, and Valdmanis 2005). Secondary data have been a rich source of information, allowing researchers to address an array of quality questions on a large scale (provincial or even national). However, because the data were constructed for a purpose other than quality measurement, and because there is wide variation in how the data are collected, such studies are potentially more prone to the various biases we have described.
Similar to the issue of research using data that were not originally collected for research purposes is that of using prospective versus retrospective data. Data that are gathered prospectively, usually to address a specific research question, are generally more accurate and more likely to provide answers to the precise question being addressed. There are relatively few research studies on quality of care in nursing homes that use prospectively gathered primary data to address a specific research question about care quality (Bates-Jensen et al. 2004; Bravo et al. 1999b; Schnelle et al. 1988; Schnelle et al. 2004), notably because they can be expensive and, in some cases, require prohibitively long follow-up periods (Gordis 2009; Rothman, Greenland, and Lash 2008). Research on care quality in residential care facilities therefore often relies on retrospective data – that is, data gathered sometime in the past and often not for the purpose of addressing a specific research question.
Partly as a result of the availability of data, researchers have become far better at measuring poor processes and outcomes as markers of bad quality. Facilities with lower rates of these poor outcomes are then classified as being of “good quality,” where “good” is defined as the absence of, or low rates of, poor quality measures (Mor et al. 2003).
Despite these methodological limits to measuring quality, there is nonetheless a relatively large body of published research that examines the relationship between the quality of care and staffing, on the one hand, and ownership, on the other. We shall briefly review these literatures in turn.
Staffing and care quality are considered to be some of the most important mechanisms for explaining observed differences in care among for-profit, nonprofit and publicly owned facilities. There is a robust and extensive US literature that describes an association between higher levels of total nursing and registered nursing (RN) staff and improved care outcomes (Bates-Jensen et al. 2004; Collier and Harrington 2008; Harrington et al. 2000b; Kramer and Fish 2001; Murphy 2006; Weech-Maldonado et al. 2004). Over the past five years numerous studies have demonstrated an association between higher overall staffing levels and both improved quality of care (Harrington 2008) and lower worker injury rates (Trinkoff et al. 2005). A small number of these studies have used prospectively gathered data.
Bates-Jensen and colleagues conducted hourly observations, mealtime observations, personal interviews and physical performance tests on over 800 residents of 34 nursing homes in Southern California. They found that after controlling for differences in residents’ level of disability, the strongest predictor of a resident being left in bed was the staffing level, with the lowest-staffed facilities being almost six times more likely than higher-staffed facilities to have over half their residents in bed. They also observed that bedridden residents were more likely to be drowsy and not socially engaged with other residents and that they ate less (Bates-Jensen et al. 2004).
Schnelle and colleagues observed 21 nursing homes in California for 16 care processes – such as regular toileting, incontinence care and repositioning – identified in the literature as important for good quality. They showed that the highest-staffed homes performed significantly better on 13 out of 16 of these processes (Schnelle et al. 2004).
An extensive study of staffing and quality was commissioned by the US Centers for Medicare and Medicaid Services (CMS) and the US Congress as a result of widespread public concern about the quality of nursing-home care. The researchers deployed a mix of observational empirical research and time-motion studies in which the precise times required to perform certain tasks (for example, toileting a resident) were measured. The report demonstrated a threshold for staffing levels below which nursing homes were more likely to experience problems with quality, such as unexplained weight loss and pressure ulcers. This threshold was 4.1 hours per resident day, consisting of 2.8 nurse aide hours (ratio of 8 patients to 1 resident care aide) and 1.3 licensed nurse hours (ratio of 18:1), of which at least 0.75 should be registered nurse hours (CMS 2001). The report further concluded that nursing protocols to support residents in washing and dressing themselves in the morning take 7 to 11 minutes. Assisting groups of residents with feeding at a ratio of 1 care aide to 3 residents is estimated to take 18 minutes (CMS 2001).
Staffing levels are clearly not the only staffing measure associated with quality of care, and a number of researchers have demonstrated an association between staff turnover and quality (Castle and Engberg 2005; Spector and Takada 1991; Zimmerman et al. 2002). However, staff turnover is itself correlated with lower RN and total nurse staffing levels (Anderson, Corazzini, and McDaniel 2004b; Harrington and Swan 2003). Other researchers have demonstrated an association between improved quality and a higher number of RNs as a proportion of total nursing staff (Castle and Myers 2006; Kim, Harrington, and Green 2009).
Another measure not directly related to staffing levels was revealed by a Statistics Canada survey of seniors living in residential care facilities. It found that one of the few determinants of how positively facility residents perceived their own health was whether they felt close to at least one staff member (Ramage-Morin 2006). Furthermore, after controlling for age, sex and chronic conditions, it was found that those who perceived their health as positive were less likely to die. Canadian research has explored how relationships between staff and residents are affected by staffing levels. In a survey of almost 1,000 direct-care staff in Ontario facilities, responders reported that more than half the time they were unable to chat with residents or provide emotional support due to time constraints. Bathing and feeding were skipped 10 percent and 20 percent of the time, respectively, for the same reason (Armstrong and Daly 2004).
Because of this strong demonstrated association between higher staffing levels and better care quality, staffing levels have become one commonly accepted measure of quality in nursing-home research. Staffing differences between for-profit and nonprofit facilities are one of the most consistent findings in the literature; numerous studies have found that nonprofit and publicly owned facilities have higher nurse staffing levels than for-profit facilities (Aaronson, Zinn, and Rosko 1994; Berta, Laporte, and Valdmanis 2005; Comondore et al. 2009; Harrington et al. 2001; Hillmer et al. 2005; McGregor et al. 2005; McGregor et al. 2010b).
Two high-quality systematic reviews on residential care facility ownership and quality have been published over the past five years. A systematic review is a scholarly attempt to assemble and review the total body of existing literature on a given topic and summarize the results. A well-conducted systematic review synthesizes the work of multiple researchers and allows the reader to draw conclusions regarding the extent of the evidence on a given topic, despite potentially contradictory results reported in individual studies (Centre for Reviews and Dissemination 2008; Liberati et al. 2009).
One of the two systematic reviews was that of Hillmer and colleagues (2005). They reviewed 38 studies of North American facilities that examined facility ownership and various measures of quality. They concluded that, overall, “residents of [for-profit] nursing homes were more likely to be recipients of poor quality compared to similar residents in [not-for-profit] facilities” (162). With respect to structural measures, they noted that nonprofit facilities had a higher staff-skill mix and lower staff turnover compared with for-profit facilities. With respect to process quality measures, the authors reported that, with one exception, all comparisons favoured nonprofit care delivery.
The other systematic review was published in 2009 (Comondore et al.). It reviewed 82 articles comparing quality in for-profit and nonprofit residential care facilities. The authors found that most studies demonstrated significantly better quality in nonprofit facilities; only three demonstrated better quality in for-profit facilities. The authors pooled the results of all studies that measured staffing levels, pressure ulcers, use of physical restraints and deficiencies reported by government inspectors. The results showed that nonprofit facilities had, on average, significantly higher staffing levels and a lower frequency of pressure ulcers. They also found there was a trend among nonprofit facilities toward less use of physical restraints and fewer deficiency citations.
Although these two reviews of quality in residential care facilities were conducted by Canadian researchers, the studies from which the data were drawn were mainly American. Only 1 of the 38 studies reviewed in Hillmer et al. and 5 of the 82 articles mentioned in Comondore et al. were Canadian. Moreover, Hillmer et al. deliberately limited the scope to North American studies. In Comondore et al., in addition to the 5 Canadian studies, only 2 others were from outside the US.
Unlike in Canada, in the US residential care is dominated by the for-profit sector. Approximately 70 percent of Medicareand Medicaid-funded beds in the US are for-profit, and 54 percent are concentrated in large corporate chains (Harrington et al. 2010a). In Canada, except in Ontario, the residential care sector is dominated by nonprofit and publicly owned facilities. This different context might produce very different results if we compare the performance of facilities by their ownership characteristics. In jurisdictions where there is a large number of nonprofit facilities, the nonprofit sector could set higher benchmarks of care quality. US research suggests that the stronger the nonprofit sector in a given market, the more likely it is that all facilities will provide better care (Grabowski and Hirth 2003).
While the relative proportion of for-profit facilities is very different in the two countries, the funding of residential care is similar, in that in both countries it is mostly public. In the US, most residential care beds are funded by Medicare and Medicaid (Wunderlich and Kohler 2001), which are government-funded insurance schemes. Medicare covers short-stay residents, often after hospital discharge, and for a limited period of rehabilitation. Medicaid funds long-stay residents who have no other means to pay for the service (Wunderlich and Kohler 2001). There are relatively few private payers in the US and Canada.
Having examined some of the differences and similarities between the residential care sectors in the US and Canada, in the next section we review the Canadian research on facility ownership and residential care quality.
One of the earliest Canadian studies on care quality in residential care was conducted by Shapiro and Tate in 1995. They used administrative data on 15,437 individuals who resided in Manitoba nursing homes from 1987 to 1991. They examined the variation in hospital admission rates for a number of diagnoses deemed by clinician experts to be “care sensitive” – that is, amenable to improvement through better care. The focus of this study was not to compare quality by ownership, but rather to assess whether administrative data might be used to monitor quality. The authors found that after adjusting for facility case mix, for-profit facilities in Manitoba were associated with higher rates of hospitalization for several care-sensitive diagnoses than were public (hospital-based) and nonprofit facilities (Shapiro and Tate 1995).
Bravo and colleagues looked at 301 randomly selected residents in 88 residential care facilities in Quebec’s Eastern Townships (1999a). They interviewed facility managers and conducted detailed resident assessments. They found that for-profit facilities ranked lower on a composite quality-of-care scale when ownership is looked at in isolation (univariate analysis). However, once other factors were accounted for, ownership lost its independent effect. The facility-level variables that were found to influence quality in the adjusted model were the number of external collaborators,3 the manager’s training, facility size and the age distribution of the residents. This study used prospectively gathered data, and its sample was much smaller than that of the Shapiro and Tate study (1995).
In Ontario, Berta, Laporte and Valdmanis (2005) analyzed Statistics Canada’s Residential Care Facilities Survey (which has surveyed all residential care facilities every year since 1974) for the period between 1996 and 2002. They reported that for-profit facilities had significantly lower levels of direct-care staff than both nonprofit and public facilities.
In British Columbia, one cross-sectional study using data from the BC Labour Relations Board examined 167 facilities (109 nonprofit and 58 for-profit), in which all staff were members of the same bargaining association and received identical wages (McGregor et al. 2005). Compared with for-profit ownership, nonprofit status was associated with an estimated 0.34 more hours per resident day provided by direct-care staff and 0.23 more hours per resident day provided by support staff after adjusting for the type of care and the size of the facility. The study also found higher levels of activity aide staffing (for leisure and recreational activities) in nonprofit compared with for-profit intermediate and multilevel facilities.4
Another British Columbia study examined the hospitalization rates for care-sensitive outcomes of approximately 43,000 individuals in residential care from April 1996 to August 1999.
The authors found that the rates of hospitalization for pneumonia, anemia and dehydration were significantly lower in nonprofit facilities than in for-profit facilities (McGregor et al. 2006). However, they also found that the overall superiority of the nonprofit sector in British Columbia was driven by facilities that were attached to acute care hospitals, were owned or operated by a health authority, or had more than one site. Single-site nonprofit (nonpublic) facilities had hospitalization rates similar to those of for-profit facilities (McGregor et al. 2006). Finally, they found that for-profit facilities – unlike nonprofit facilities, which varied in performance – had uniformly higher hospitalization rates, regardless of whether they were single-site, multisite or part of a large corporate chain.
Doupe and colleagues used administrative data from Manitoba to assess a number of quality indicators (Doupe et al. 2006). They found higher rates of falls, pressure ulcers, respiratory infections, fluid and electrolyte imbalances, poly-pharmacy (excessive number of medications), and benzodiazepine and antipsychotic use among residents in for-profit facilities in the Winnipeg region than among those in nonprofit and public (hospital-attached) facilities, after adjusting for case mix and other potential confounders. They found no significant differences in staffing levels between for-profit and nonprofit facilities.
A more recent longitudinal British Columbia study using staffing data from the Statistics Canada Residential Care Facilities Survey found that both nonprofit and publicly owned facilities had higher levels of total nurse staffing hours per resident day (licensed practical nurse, RN, care aide) than for-profit facilities, after adjusting for facility size, resident age, sex and case mix (McGregor et al. 2010b). The same study also found that average staffing hours in all facility groups had increased over time. However, the rate of increase in total nurse staffing hours was significantly higher in public facilities than in the other ownership groups.
Biomedical science increasingly identifies significant associations between various exposures and outcomes. However, the fact that a correlation or association between two factors is demonstrated does not mean that the presence of one factor causes the other. For instance, an editorial published in the British Medical Journal at the time of the most recent systematic review by Comondore and colleages (2009) argued that, in spite of the evidence demonstrating a correlation between publicly funded for-profit care delivery and inferior quality, we cannot infer causation (Konetzka 2009). Failing to understand the complexity of these relationships prior to assuming causation can lead to erroneous conclusions (Gordis 2009; Rothman, Greenland, and Lash 2008).
In the biomedical sciences, a well-designed, randomized, controlled trial is generally considered to provide the most solid evidence for establishing causation (Guyatt et al. 2008; Gordis 2009; Strom 2005). In this type of trial, participants are randomly assigned to an experimental group or a control group and are typically blinded as to which group they are in (Gordis 2009). A common example of this occurs in drug trials, where participants are given either the active drug or a placebo (an inactive or fake drug) and not told which one it is. The possible outcomes of the treatment are predefined and the participants’ responses to the treatment are measured, ideally by individuals who are also blinded – that is, not told whether the participants have been given the active drug or a placebo. Finally, the results from both groups are compared (Gordis 2009; Strom 2005).
While this model for establishing causal evidence can work well for drug testing, it usually cannot be reproduced in the area of health services research (Gordis 2009). For example, it would be ethically and technically difficult to design a double-blinded, randomized, controlled trial of two groups of facilities with similar residents, funding, size and location. Moreover, it would require that one group of facilities be randomly assigned to ownership by one or more for-profit organizations and the other to ownership by public or nonprofit organizations. Finally, those collecting and analyzing the results would have to be blinded as to which group the results originated from and, to the extent possible, all potential biases would have to be controlled for.
Given the type of research question they would pose (“Does for-profit ownership cause lower quality in residential care facilities?”), it is unlikely that such trials would ever be conducted. Moreover, health policy issues such as this, with their multiple contextual factors, are probably too complex for a clinical trial to address (Bell 2010).
In the absence of evidence from randomized controlled trials, the epidemiologist Sir Austin Bradford Hill produced a series of criteria for evaluating the conditions under which researchers can “pass from an observed association to a verdict of causation” when assessing observational studies (1965, 295). In what follows we review each of these criteria and assess the extent to which they are present in the research on ownership and quality.
The strength of the association is the magnitude of the difference between (usually) two groups: if the magnitude of statistically significant differences is large, the relationship is more likely to be causative. What this means in statistical terms is usually expressed as a risk ratio, rate ratio or odds ratio (that is, the odds of something occurring in one group compared with the other). If, for example, the odds ratio is much greater or much less than 1 and statistically significant – that is, the difference is unlikely to have occurred by chance alone – then there is a more convincing argument for causation (Gordis 2009).
In the case of differences between the quality in for-profit and that in nonprofit or publicly owned residential care facilities, the magnitude of difference depends on the quality indicator being measured. The effect magnitudes described by Comondore and colleagues in their systematic review – a relative increase of 11 percent more staffing hours and an 8.4 percent reduction in pressure ulcer prevalence (2009) – appear small compared with differences observed in the biomedical world. In occupational and environmental epidemiology, for example, arguments for a causal association between an exposure and an outcome may be considered strengthened by a twofold greater risk seen in the exposed group compared with the non-exposed group. This is because the stronger an association, the less likely it is that the results will be overwhelmed by residual bias, or confounding (Gamble 2010).
Relative to these paradigms, the differences observed in studies comparing for-profit and nonprofit care quality are modest. However, it should also be noted that in policy research, small differences often apply to large numbers of people, so that these differences become magnified. In the case of facility ownership and staffing levels, while they acknowledge the challenge of proving causation using observational studies, Comondore and colleagues calculated that the pooled difference of 0.42 hours of care per resident per day in publicly funded nonprofit facilities compared with for-profit facilities, applied to the distribution of for-profit facilities in Canada, means that facility residents would receive 42,000 additional hours of care per year if these services were provided by nonprofit facilities. Similarly, the authors estimate that 600 of 7,000 residents in Canada and 7,000 of 80,000 residents in the US have pressure ulcers attributable to for-profit ownership (Comondore et al. 2009). In other words, the demonstrated positive effect of ownership on quality in most studies is relatively small. However, when applied to large-scale health care systems, the real effect can be substantial.
A second criterion by which to judge whether the evidence supports causation, the consistency criterion, may be expressed by the question, “Has the association been repeatedly observed by different persons, in different places, circumstances, and times?” Different methodological approaches to the question that yield the same answer further strengthen the consistency criterion for causation (Hill 1965).
The relationship between ownership and residential care quality has been examined across a large number of jurisdictions in the US, with data from Pennsylvania (Aaronson, Zinn, and Rosko 1994), California (O’Neill et al. 2003), Maryland (Zimmerman et al. 2002) and the US as a whole (Castle 2000a; Harrington et al. 2001). Studies from a number of Canadian provinces (Berta, Laporte, and Valdmanis 2005; Doupe et al. 2006; McGregor et al. 2005; McGregor et al. 2006; Shapiro and Tate 1995), from Taiwan (Lee et al. 2002) and from Australia (Pearson et al. 1992), while fewer in number, have also demonstrated a significant association between publicly funded for-profit delivery and care of inferior quality.
This association between for-profit status and inferior quality has been demonstrated using a variety of facility-level data sources (Aaronson, Zinn, and Rosko 1994; Castle and Fogel 1998; Davis 1993; Harrington et al. 2001; Spector, Selden, and Cohen 1998) and individual-level primary (Pearson et al. 1992) and secondary data sources (Grabowski and Angelelli 2004; Grabowski and Stevenson 2008; McGregor et al. 2006; Stevenson 2005). While most studies have used large administrative data sets, some are based on data that were gathered prospectively to answer a specific research question (Lee et al. 2002; Pearson et al. 1992), and some have used qualitative methods (Baumbusch 2008). Except in a minority of studies, the direction of the association between for-profit facility ownership and inferior quality is consistent.
Beyond consistency of results across jurisdictions using a variety of data sources and methodologies, consistency has also been observed across a wide range of quality measures. Research has found that for-profit ownership is associated with lower staffing levels (Aaronson, Zinn, and Rosko 1994; Berta, Laporte, and Valdmanis 2005; Harrington and Swan 2003; McGregor et al. 2005; O’Neill et al. 2003); higher rates of pressure ulcers (Comondore et al. 2009), hospital admissions (Grabowski et al. 2008; Konetzka, Spector, and Shaffer 2004; McGregor et al. 2006; Shapiro and Tate 1995), deficiency citations for use of restraints (Castle 2000b; Zinn et al. 2005) and complaints (Stevenson 2005, 2006); and is a factor in a variety of other global quality measures (Gray and McNerney 1986; Pearson et al. 1992).
In summary, there is considerable consistency in the research pointing to an association between nonprofit ownership and superior quality.
Temporality means that cause must precede effect. Cross-sectional studies – that is, studies in which data on exposure and outcome are measured at the same point – are generally limited in their ability to demonstrate a temporal association (Gordis 2009). Thus cross-sectional studies typically cannot establish whether for-profit residential care facilities attract a higher volume of residents who already have pressure ulcers, experience falls or submit complaints, or whether residence in such facilities actually results in a higher frequency of these outcomes.
Grabowski and Stevenson reviewed US nursing-home performance after nonprofit facilities converted to for-profit, and vice versa. They used OSCAR nursing-home data combined with individual-level clinical data from RAI-MDS on care quality collected by the CMS (Grabowski and Stevenson 2008). The authors examined staffing levels, serious deficiency citations and care quality indicators in facilities that changed ownership status between 1993 and 2004. They found that the performance of facilities that had converted from for-profit to nonprofit status had already begun to improve before the ownership change. Conversely, facilities that converted from nonprofit to for-profit status demonstrated a deterioration in performance before the change in ownership.
Banaszak-Holl and colleagues examined the effect of acquisition by chain facilities and, similarly, found that chains tended to acquire poorer-quality nursing homes. They also found that while a facility’s quality declined immediately following its acquisition by a chain, the longer-term performance of an acquired facility was influenced by the chain’s performance before the acquisition (2002).
Because of this tendency for poorer-quality nonprofit facilities to convert to for-profit status, it has been difficult, methodologically, to measure or estimate the independent effect of facilities’ for-profit status after conversion. In a recent paper, Bowblis deliberately controlled for the status of facilities before conversion (2009). After adjusting for this and other potential confounders, Bowblis reports that converted for-profit facilities had higher rates of pressure ulcers but lower rates of restraint use after conversion.
In another study assessing temporality, Amirkhanyan examined the effect in the US of residential care facilities converting from publicly owned to for-profit status. The author found that these facilities had, on average, 46 percent more deficiencies than those that remained publicly owned. In contrast, similar changes were not seen in facilities that converted from public ownership to nonprofit status (Amirkhanyan 2008). Paradoxically, the same study found decreased rates of accepting Medicaid residents among facilities converting from for-profit to nonprofit status. This decrease may be due to higher staffing standards in nonprofit facilities that cannot be sustained by the lower funding levels provided for Medicaid residents.
To sum up, there appears to be some evidence to suggest the existence of a temporal link between conversion of residential care facility ownership to for-profit status and a decrease in quality for some outcomes.
The concept of dose response (or biological gradient, as defined by Hill [1965]) refers to a doseresponse effect whereby the greater the exposure to the causative agent, the greater the effect of a given outcome. The fact that the death rate from lung cancer increased linearly in relation to the number of cigarettes smoked is an example of biological gradient. In the case of ownership and quality, while there is nothing biological about the issue, one can nonetheless ask whether a gradient effect between profit and quality has been demonstrated.
Harrington and colleagues have completed several studies on the performance of large forprofit residential care nursing-home chains in the US (Harrington et al. 2010b; Harrington et al. 2010c). The authors note that such chains were developed to maximize shareholder value, resulting in choices that prioritize this goal and subordinate others. In one of the studies, the authors found that the 10 largest chains, representing 14 percent (238,745) of all beds in the US, had 14 percent lower RN staffing and 9 percent lower total nurse staffing than the US average for the 2003-08 period. Most had a history of numerous federal citations and enforcement actions for poor care. Although the authors didn’t perform direct calculations to determine the correlation between these companies’ profit margins and measures of poor care, they note that all the chains were financially successful. Their assets ranged from $400 million to $8.45 billion, and their long-term debt-to-total-assets ratios ranged from 14 to 72 percent.
O’Neill and colleagues examined nursing-home data from 1,098 facilities in California to assess the relationship between profit and the quality of care in nursing homes. They found that forprofit facilities in the group with the highest profit margin had significantly more deficiencies than those in the next-lowest profit group. Those in the highest-profit group were also found to have more serious deficiencies than the ones in all the lower-profit groups, after controlling for resident case mix and other facility and market characteristics (O’Neill et al. 2003).
O’Neill and colleagues’ findings suggests the presence of a gradient effect, where progressively greater profit resulted in progressively poorer quality.
The ability to demonstrate the mechanism through which an association exists, or its plausibility, is another criterion for establishing causation. Perhaps the most obvious mechanism whereby for-profit ownership produces lower quality is the employment of fewer nursing staff. As discussed earlier, one of the strongest predictors of improved quality of residential care is higher staffing levels (Bates-Jensen et al. 2004; Castle 2009; Castle and Engberg 2007; Harrington et al. 2000b; Konetzka, Stearns, and Park 2008; Kramer and Fish 2001; Murphy 2006; Schnelle et al. 2004; Weech-Maldonado et al. 2004). US and Canadian research has shown that for-profit facilities hire fewer nursing staff, which results in lower-quality care (Aaronson, Zinn, and Rosko 1994; Berta, Laporte and Valdmanis 2005; Comondore et al. 2009; Harrington et al. 2001; Hillmer et al. 2005). For-profit facilities have also been found to pay their staff less (Harrington et al. 2010c).
The plausibility of this finding (of lower staffing levels in the for-profit sector) is presumably due to the fact that the organizational goal of these facilities is profit generation. Decisions to hire fewer staff or not to replace staff who are ill or on vacation are strategies for cutting what is the most costly line item. O’Neill and colleagues describe the relationship as follows: “If increasing quality raises costs more quickly than it does revenues, profits must fall as quality improves. That is, a trade-off between profit and quality would exist” (O’Neill et al. 2003, 1319).
Another possible mechanism through which the nonprofit quality advantage might come into play is related to the greater amount of social capital associated with nonprofit enterprises: the capacity to mobilize volunteers who provide companionship to residents and who raise funds for capital equipment to enhance care. Furthermore, nonprofit societies are often given tax breaks not available to the private sector, thus enabling them to put more resources into direct resident care. In conclusion, Hill’s plausibility criterion is present and has been described by a number of authors.
When similar effects have been observed in a different context there is an analogy with that context. In sectors other than residential care, there is solid evidence that care delivered by nonprofit acute care hospitals, hemodialysis clinics and ambulatory care clinics (Devereaux et al. 2002a; Devereaux et al. 2002b; Himmelstein et al. 1999) is overall of better quality than that delivered by corresponding for-profit facilities. Outside of the health sector, studies looking at the daycare sector in Quebec (Japel, Tremblay, and Côté 2005) and Canada (Cleveland et al. 2008) have found a similar quality gap between for-profit and nonprofit ownership. It is therefore reasonable to conclude that the criterion for analogy is present in the literature.
There is coherence to the association if there is supporting evidence from other, less direct sources. The equivalent in the ownership/health-policy paradigm is difficult to conceptualize, except that the association between profit generation and inferior quality should not seriously conflict with the generally known facts of the relation between the two. As described in relation to the analogy criterion, the association of publicly funded for-profit delivery and inferior service quality has been described in a number of settings in health care and other services. The association of for-profit delivery in residential long-term care and inferior quality does not appear to conflict with the generally known facts, and one can therefore conclude that coherence is present in the literature.
If a change in outcome can be demonstrated by a change in exposure, a causal association is much more likely to exist. It is unlikely that randomized trials to assess the effect of for-profit ownership on quality will ever be conducted. Research on this question therefore has to rely on the natural policy experiments performed by measuring the effects of policy changes relating to ownership and/or comparing quality across different ownership types in different contexts.
When the causative agent results in very specific effects, we say there is specificity in the association. This criterion is more relevant to a biomedical paradigm (versus a health systems or policy paradigm): for example, the assumption that mesothelioma, a very specific type of lung cancer, is seen only when an individual has been exposed to asbestos (Britton 2002). While the concept is of limited application in the health policy arena, the strongest empirical evidence exists for the association between for-profit status and lower staffing levels. Since the number of staff hired is also the most costly line item and has the greatest likelihood of affecting profit, one might argue that there is some degree of specificity in the association.
In his original work Hill emphasizes that these nine criteria should be considered not as necessary prerequisites for causation, but rather as a framework for weighing the evidence for and against causation: “All scientific work is incomplete – whether it be observational or experimental. All scientific work is liable to be upset or modified by advancing knowledge. That does not confer upon us a freedom to ignore the knowledge we already have, or to postpone the action that it appears to demand at a given time” (1965, 300).
The evidence demonstrating the relation between for-profit ownership and lower care quality appears to meet many of the criteria for a causal association, especially those of consistency, dose response, plausibility and analogy. While the magnitude of the effect is not great, when it is applied to large-scale health care systems, the real effect can be substantial. There is also some evidence that observational studies meet the criteria for a temporal association. Although Canadian research to date generally supports the generalizability of the US findings, there is a need for more research from all provinces in Canada and from other countries to confirm this.
Finally, the establishment of a causal link between for-profit facility ownership and inferior care does not mean that all for-profit facilities provide poor care. In the same way that not all smokers get lung cancer, many for-profit facilities provide good care. However, the evidence suggests that as a group they are less likely to provide good care than nonprofit or public facilities. It would therefore be prudent to ensure that public policy reflects this evidence.
In the previous section, we summarized the evidence on residential care facility ownership and quality. We found there is a growing body of evidence confirming an association between for-profit ownership and inferior quality care, and there is evidence suggesting a causal link between for-profit ownership and poorer quality.
Unfortunately, the policy decisions taken in many provinces over the last decade or so appear to run counter to the research evidence. Indeed, while the majority of facilities are still public or nonprofit in all provinces except Ontario, there are wide variations across provinces (see table 5), and the share of the for-profit sector has been growing in several provinces.
Why this inconsistency? While it is not the purpose of this study to analyze in depth the political and economic context that moved policy in this direction, we briefly review the factors that may have contributed to it in the following section.
Several factors have contributed to increase the role played by the private sector in residential long-term care. First, Canadian governments have failed to keep up with investments in public infrastructure over the recent decades for not only roads and bridges, but also hospitals and residential care facilities (TD Bank Financial Group 2004; Harchaoui, Tarkhani, and Warren 2003; Mackenzie 2004). Canada’s public asset base has been falling behind year after year for more than 30 years. There has thus been a substantial backlog in demands to repair and renovate older buildings and equipment and to build new ones. In fact, the Toronto Dominion Bank estimates that the infrastructure gap, while difficult to measure precisely, “is massive” and could be as “high as $125 billion or 6 to 10 times annual investment flows” (TD Bank Financial Group 2004, 5).
This pressure on governments to address the infrastructural gap is also increasing due to our aging population and the need to increase the number of residential care beds. In addition, individuals in residential care are more disabled than they were a decade ago (CHA 2009; Frohlich, De Coster, and Dik 2006), which presents greater challenges to those designing new facilities and upgrading old ones. Safety standards and building codes have also changed. Many provinces have stricter standards; rooms must meet the physical needs of disabled residents (British Columbia 2009). As a result, governments must now find additional sources of financing to address this demand and have sought nontraditional ones, notably by partnering with the private sector.
The second factor contributing to the observed policy paradox is the gradual devolution of responsibility for public capital investment from federal to provincial and local governments, without the necessary transfers or tax room to support it (Mackenzie 2004; Gagné et al. 2006). Indeed, in 1961, the federal government owned 39 percent of the Canadian public capital stock, the provinces 35 percent and local governments 26 percent. Forty years later, in 2002, the federal and local governments had virtually reversed their positions: the former owned almost 18 percent of the stock and the latter 48 percent (Harchaoui, Tarkhani, and Warren 2003). The resulting budgetary pressure on local and provincial governments to raise sufficient money to maintain the existing capital stock and to allocate money for new investments has thus increased over time (Mackenzie 2004).
A third factor that came into play was the fight against budget deficits and the debt aversion that developed in the 1990s. This, combined with competitive pressures to lower the tax burden, encouraged governments to avoid large-scale public borrowing to finance necessary but costly infrastructure. Getting into debt was considered a bad political move up until 2009, when governments showed a willingness to run deficits again in order to finance fiscal stimulus packages to deal with the global financial crisis (IMF 2009).
The fourth factor behind the policy paradox relates to the introduction of new accounting standards during the 1990s. This added an additional barrier to public borrowing. Under these new rules, governments were no longer able to keep capital expenditures off their books by delivering capital projects through government agencies (such as universities or hospitals). Accounting rules allowed governments to amortize their capital expenditures over the economic life of the assets, but only in the case of capital expenditures for which they were directly responsible. Because much of Canada’s infrastructure has traditionally been financed through transfers, the effect of these changes was to force governments to account for these capital expenditures as if they were current expenditures (Mackenzie 2004). For example, if the federal government made a transfer payment to a province to support the construction of a new water facility, it had to be recorded as a one-time expense, which suggested that government had incurred a huge debt, in contrast to the previous practice of treating the payment as a long-term investment amortized over many years. In the climate of the 1990s and early 2000s, governments wished to avoid the accusation of piling up debt at all costs.
It is in this context that governments started to turn to the private sector and consider publicprivate partnerships (P3s) to finance some of their obligations. Under P3s, a government contracts with a private company to construct new infrastructure, and in some cases to provide some or all of the services for that new infrastructure once it is completed. Often the contracts are long term, sometimes lasting more than 30 years. In the case of residential care facilities financed through a P3, the private partner often assumes service delivery once the new facility is built. An example of this is the 200-bed facility in St. Lambert, on Montreal’s South Shore. Thus the financing of new residential care beds through P3 arrangements is intimately linked to the expansion of for-profit delivery.
While P3s still only account for 10 to 20 percent of all infrastructure spending in Canada, they are nevertheless a key tool that governments now count upon to help address the infrastructure gap (Iacobacci 2010). In fact, British Columbia (Partnership BC), Ontario (Infrastructure Ontario), Quebec (Agence des partenariats public-privé du Québec, now Infrastructure Québec) and Alberta (Capital Financing Office) as well as the federal government (PPP Canada) have all set up agencies to support the development of these partnerships. Municipalities are also involved in this type of transaction.5 According to Ernst and Young, at least 100 P3s have been signed in Canada since the early 1990s – of which a third are in the health care sector, including several long-term care facilities – and they amount to about $20 billion in investment (Ernst and Young Orenda 2006).
Some provinces, such as British Columbia and Ontario, have also introduced a new request for proposal (RFP) process for organizations that want to bid on government contracts (Cohen et al. 2005). In addition, British Columbia has phased out infrastructure support to nonprofit agencies. Without such support, which often takes the form of technical expertise necessary to submit competitive bids, nonprofit agencies may be prevented from bidding on contracts. Thus the introduction of a competitive RFP process has further contributed to the expansion of for-profit-delivered residential long-term care over the last decade (CUPE 2009) – despite the growing empirical evidence that this sector is likely to deliver inferior care.
Many have argued that improving government regulation could counter the quality concerns associated with expanding for-profit care delivery.
The residential care population is one of the most vulnerable groups in our society, and the residents and their families have little voice (Cohen et al. 2005) and little option for exit (Hirth 2009). Consequently, regulation of the quality of care and adequate enforcement of regulations to ensure minimum staffing levels and other quality indicators are fundamental. Facilities that care for this population need to be licensed,6 and there should be regular unannounced inspections by trained inspectors and good information systems for reporting on quality measures.
However, while good regulation is important in any setting, it is not a panacea. Without the financial and human resources required to implement it and monitor it, improved regulation may not be as effective as expected, especially in for-profit settings.
Kieran Walshe outlines two very different approaches to regulation (2001). “Deterrence” regulation views the organizations being regulated as having “bad intentions” and being out to “break the rules.” This approach is punitive, sanctions-oriented and usually more costly, as the regulated organizations become defensive, thereby undermining the goals of regulation. “Compliance” regulation views the organizations being regulated as basically well intentioned. This approach uses less formal and more supportive ways to regulate.
According to Walshe, the more profit generation is the organizational goal of long-term care institutions, the more compliance must be replaced with a deterrence style of regulation. Deterrence, however, is costly and diverts money away from providing direct care for the residents. In the US, which has one of the most highly regulated systems, the annual cost of certifying nursing homes is estimated to be about $22,000 per facility, or $208 per bed (Grabowski and Castle 2004).
Moreover, the research evidence on the effectiveness of regulation in ensuring a high quality of care is meagre, and the little evidence that is available is mixed. On the one hand, research from the US has demonstrated that the number of state fines collected for inspection violations is inversely related to the number of facility complaints per nursing-home bed, suggesting that better regulation and enforcement does influence quality (Harrington et al. 2008). On the other hand, a recent study of a sample of regulated and unregulated nursing homes in Quebec concluded that regulation had little impact on life expectancy (Bravo 2002). In fact, while everybody agrees that regulation is necessary, there is “too little evidence to be able to determine whether the benefits justify the costs,” and there is clearly a need for more research in this area (Walshe 2001, 141).
All in all, we doubt that regulation alone can counter the negative outcomes associated with for-profit organizations – or if it can, it would be at a very high cost that would divert resources away from care delivery itself. As Walshe points out “when regulatory objectives and market pressures collide, as they do for nursing homes, organizations will often attempt to reconcile the conflicting pressures, but ultimately the stronger market pressures are likely to prevail” (2001, 140). If the for-profit sector continues to expand in Canada these conflicting pressures will increase, creating bigger challenges for regulatory bodies.
In that context, we recommend that services be funded and delivered by the public sector and nonprofit organizations. It is beyond this study’s scope to suggest detailed solutions to the current misalignment of policy with evidence, but in the following section we sketch out several policy suggestions that decision-makers may wish to consider to support the role of nonprofit organizations in the delivery of services and to secure the quality of services delivered. Some of these are clearly more challenging than others to implement.
In addition, interested readers can refer to the appendix where the recommendations from five major Canadian reports on long-term care published within the last two years are summarized.
If public policy is to align itself with the research evidence that supports care by nonprofit and/or publicly owned institutions, a key challenge will be to expand the residential care sector using publicly funded capital investment.
While many provinces have been using P3s to expand capacity in this sector, a number of recent initiatives suggest that some governments are beginning to look at other options. For example, Alberta has issued government bonds that can be used in the construction of new residential care facilities (“Alberta Bonds” 2009), and Prince Edward Island has decided to expand its residential care facilities using traditional public funding (CUPE 2009).
Competitive bidding through RFPs favours larger for-profit corporations, which have the necessary infrastructure to compete (Cohen, Tate, and Baumbusch 2009). Provincial governments could develop support programs that offer expertise to nonprofit societies to enable them to make their bids more competitive.
There is an example of such government support in British Columbia. In the 1990s the Hospital Planning and Construction Division of the Ministry of Health provided comprehensive technical support to nonprofit organizations. Specific support included recruiting architects or engineers and project managers, signing off on preliminary and final construction drawings, reviewing tenders, approving the awarding of contracts, attending project management meetings and approving contract payments.
The main strength of this system was the transparency of the process – the scoring system for projects, the reasons why one bid succeeded while another did not, and the fact that information was publicly accessible. Mount St. Mary, a 200-bed residential long-term care facility in Victoria, is a good example of a capital construction project that received technical and infrastructure support. The design, construction and costs for this facility were deemed very successful.7
Unfortunately, despite its demonstrated success, infrastructural support to nonprofit organizations in British Columbia ended in 2001, and since that time, virtually all new residential long-term care beds in that province have been in the for-profit sector.
The US has developed a number of interesting methods to encourage the expansion of residential care in the nonprofit sector. For example, some states have loan programs for nursing homes that are designated for nonprofits. As well, the US Department of Housing and Urban Development provides loan guarantees for nursing homes (Such et al. 1996).
In Canada, since 2006, Infrastructure Ontario has offered a program of affordable financing to nonprofit long-term care residences to renovate or improve existing facilities and construct new ones. As of August 2010, loans worth a little over $100 million had been approved (Infrastructure Ontario 2010). The Canada Mortgage and Housing Corporation, in partnership with its provincial counterparts for social housing development (for example, AccèsLogis Québec), could play a role by developing a program to support the construction of new residential care beds in the nonprofit sector.
One of the principal ways that high profit margins are generated in the residential care sector is by instituting lower staffing levels, which result in inferior quality of care. Research evidence (Bostick et al. 2006; Castle 2009; CMS 2001; Schnelle et al. 2001; Schnelle et al. 2004) and reports on the residential care sector from a range of stakeholder constituencies have emphasized this (CHA 2009; CUPE 2009; Cohen et al. 2005; Cohen, Tate, and Baumbusch 2009; PriceWaterhouseCoopers 2001; Sharkey 2008).
Legislating minimum staffing levels would be a key strategy for improving quality. This approach is used in other institutional contexts; for example, many jurisdictions set minimum student-teacher ratios in education and minimum staff-child ratios in daycare. Similar minimums could be applied for this frail population of seniors, which is arguably as vulnerable as the populations in schools and daycares. Research has demonstrated that in jurisdictions where such minimums have been implemented, staffing levels are higher (Harrington, Swan, and Carrillo 2007) and restraint use and inspection deficiencies have declined (Park and Stearns 2009).
The US literature has identified a benchmark of a minimum of 4.1 nursing hours per resident day, below which residents are more likely to experience harmful effects such as pressure ulcers and unexplained weight loss (CMS 2001; Harrington et al. 2000a). Research on the generalizability of these benchmarks in the Canadian context is urgently needed (Cohen, Tate, and Baumbusch 2009).
In most Canadian for-profit and nonprofit facilities (although not in the publicly owned facilities), nursing hours fall below 3.5 hours per resident day (Berta, Laporte, and Valdmanis 2005; Doupe et al. 2006; McGregor et al. 2005; McGregor et al. 2010b. Therefore, setting a minimum staffing standard of 3.5 nursing hours per resident per day would be a reasonable first step.
Legislated minimum benchmarks for staffing in residential care are insufficient on their own to improve staffing levels. Adequate funding to support these benchmarks must be available and ongoing. The cost of this could be offset, in part, by reduced costs related to hospitalizations, pressure ulcers, higher turnover and the workers’ compensation claims associated with lower staffing levels.
In the US, the cost to Medicare of short-stay facility residents being readmitted to hospital within 30 days of discharge was estimated at US$4.34 billion in 2006 (Mor et al. 2010). In residential care, the cost of treating people for pressure ulcers in one year was more than $800 million. The cost to facilities of staff turnover was estimated to be $2,200 to replace one care aide and $7,000 for an RN (Castle and Engberg 2005).
While similar Canadian data are not available, the findings are unlikely to differ substantially in the Canadian context. Therefore the cost of increasing public funding to support higher levels of facility staff would at least in part be mitigated by savings in other parts of the system.
Public funding in many provinces is global. Facilities thus have some discretion as to the amounts they apportion to direct care, other staff, building maintenance and property costs. This presumably allows them greater discretion to hire fewer staff or to not replace individuals who are sick or on vacation. Targeting funding for direct-care staff, which must be returned if it is not spent for this purpose, is a mechanism by which to ensure that public funds given to facilities are spent on direct resident care. This funding feature is already in place in Ontario. However, whether it has decreased the variation in staffing levels across facilities has yet to be evaluated.
Canadian research evidence in British Columbia suggests that nonprofit residential care delivered by organizations in larger groupings – either attached to a hospital, part of a health region, or part of a larger network – is more likely to result in fewer hospitalizations for caresensitive outcomes (McGrail et al. 2007; McGregor et al. 2006). There is also some evidence that overall care quality is better in nonprofit facilities that are part of larger organizational entities (Bravo et al. 1999a). Policies that encourage larger networks of nonprofit facilities and the affiliation of such facilities with academic institutions (Rantz et al. 2003; Kirkevold 2008) and regional health authorities are likely to result in improved quality.
There is good empirical evidence that leadership that fosters the improvement of quality results in better public service (Boyne 2003). Studies in the nursing-home setting support this finding (Rantz et al. 2004). A culture of greater involvement by care aides in team decisions has been found to be associated with greater staff retention (Glouberman et al. 2007 ), fewer worker compensation claims (Yassi et al. 2004) and improved resident outcomes (Barry, Brannon, and Mor 2005). The Institute for Healthcare Improvement is a nonprofit society in the United States that has developed an expertise in supporting health care quality improvement with many excellent results. If Canada’s residential long-term care sector becomes more involved with this or an equivalent structured quality improvement initiative, quality is likely to improve.
When facility residents are ill or injured, they are often transferred to the nearest acute care hospital for additional care and/or investigation. Being transferred to hospital often has negative effects; it can cause residents’ quality of life to decline further by increasing the risk of pressure sores (Allman et al. 1986), delirium and falls (Gillick, Serrell and Gillick 1982). Furthermore, there is now some evidence that treating residents in place for conditions like pneumonia may produce better outcomes (Fried, Gillick and Lipsitz 1997). In many jurisdictions, the budgets and organization of acute care and residential long-term care are kept separate, and as a result, mutual accountability is lacking. Facilities are accused of abandoning responsibility for sick residents by sending them to hospital. Hospitals are accused of discharging residents back to their facilities before they are fully stabilized. Policies that support closer alignment between the two sectors would enable better communication and accountability between them and thus improve care quality (Institute for Healthcare Improvement 2010). Quebec has begun to integrate the two sectors, and an evaluation of the successes and failures of this integration would be useful (Levine 2005).
Some countries, such as Norway, have teaching residential care homes where students of nursing, medicine, gerontology and other disciplines are sent for practical experience (Kirkevold 2008). These are also research sites for academics who are interested in aging and facility care. Preliminary evaluation of this Norwegian program has been positive, and it has resulted in improved quality of care, presumably due to the increased interest and attention paid to these issues and the exchange of ideas resulting from such partnerships. The CHA and some authors in the US have called for more partnerships between academic programs and long-term residential care facilities (CHA 2009; Mezey, Mitty, and Burger 2008).
The type of training and allocation of resources in residential long-term care do not, generally, deal adequately with end-of-life issues. Palliative care services are often inadequately integrated into residential long-term care, and staff and physicians are often unprepared to discuss end-of-life wishes and expectations with residents and their families. A British Columbia study found that one in four deaths among residents of free-standing (not attached to a hospital) residential long-term care facilities still occurs in hospital (McGregor et al. 2007). A survey done in one British Columbia health region found that less than half of all facilities had implemented medical and nursing protocoles for palliative care (McGregor et al., 2010a).
A number of recent Canadian reports have drawn attention to the need for improved end-oflife care for this population (CHA 2009; CUPE 2009; Cohen, Tate, and Baumbusch 2009).
Almost every report on residential long-term care has called on governments to make public information about the quality and accessibility of facilities (CHA 2009; CUPE 2009; K. Carter 2009; Cohen, Tate, and Baumbusch 2009). A BC ombudsman’s report calls for a Web site that would provide information on the funding, ownership, resident costs and staffing of facilities (K. Carter 2009). It also calls for information to be publicly available on the direct-care staffing levels of RNs, LPNs and care aides; the number of direct-care hours provided per resident per day; the number and qualifications of direct-care staff scheduled for each shift; access to physicians and other health professionals; the number of occupational therapists, physical therapists and similar staff; and the languages spoken by care providers (K. Carter 2009).
Ontario has so far developed the most extensive system of public reporting. The Ontario Ministry of Health hosts a Web site (https://publicreporting.ltchomes.net/en-ca/default.aspx) that provides information on facilities, including the type of operator; the number of beds; the date of the last inspection; and the number of verified complaints, citations and unmet standards (Ontario MOHLTC 2009). British Columbia is also moving toward this type of public reporting; however, it has been up to the various regional health authorities to post their data, and access to them varies considerably by region. Moreover, there is no requirement for either consumer complaints or staffing levels to be publicly posted, despite the fact that the ombudsman’s report calls for public reporting of this information (K. Carter 2009).
The US has developed a national reporting system whereby all Medicareand Medicaidfunded facilities are listed on a publicly available Web site (CMS 2010). The public can access routinely updated information on each facility’s staffing levels and complaints history, and facilities are given a star rating based on their performance on a number of quality indicators.
While this is not a guarantee of quality, it is hoped that public access to agreed-upon quality measures will encourage greater accountability on the part of facilities and governments and lead to better care for their vulnerable populations.
Complaints, rates of pressure ulcers and staffing levels, while important to measure, are proxy indicators of care quality. The best measure of quality may well be the residents’ and their families’ perception of the care they receive. Families and residents should be invited to complete surveys at regular intervals, thereby providing facilities and the public with continuous feedback. Facility participation in the survey process should be a mandatory part of licensing.
Such a survey has been developed for primary care settings in the US and parts of Canada and has been used successfully. The anonymous survey, entitled “How’s Your Health?,” consists of questions that reflect a wide range of quality measures such as access to and continuity and coordination of care (Wasson et al. forthcoming). The data are collected by Dartmouth University, and the results are sent back to primary care providers to inform them of the strengths and weaknesses identified by survey respondents.
A similar survey developed for residential care settings could be a powerful means of putting residents and families at the centre of quality improvement.
While Canadian research suggests that there is considerable variation in quality within the nonprofit residential long-term care sector that we need to better understand, there is sufficient empirical evidence in the peer-reviewed literature to conclude that providing public funding for residential long-term care to for-profit facilities is likely to produce inferior outcomes. The causal link between for-profit facility ownership and inferior care does not imply that all forprofit facilities provide poor care, but the evidence suggests that, as a group, such facilities are less likely to provide good care than nonprofit or public facilities. It would therefore be prudent if public policy reflected this evidence.
The policy direction in many provinces, however, seems to run counter to the research findings, with the apparent growth in publicly funded, for-profit residential care. One reason for this is governments’ reluctance to finance the construction of new facilities by incurring debt, and turning instead to public-private partnerships (P3s) to build residential long-term care facilities. Since the private partner often assumes responsibility for service delivery once a P3 facility is built, the financing of new residential care beds through P3 arrangements is intimately linked to the expansion of for-profit delivery, which is inconsistent with the evidence on ownership and quality.
We recommend that new residential care capacity be kept within the public and nonprofit sectors. Policies to enable this include providing traditional public sector funding; raising capital through the sale of government bonds; making low-interest loans available through government housing agencies such as the Canada Mortgage and Housing Corporation and AccèsLogis QueÌbec; and providing infrastructural and technical support to enable nonprofit organizations to make competitive bids on new projects. However, nonprofit or public delivery of residential care is not sufficient on its own to ensure high quality care for frail elders. It merely provides the most conducive environment for implementing other key policies that foster quality.
Adopting legislated minimum staffing levels in residential long-term care – just as many Canadian jurisdictions set minimum student-teacher ratios in education and minimum staffchild ratios in daycares – would be an important measure to improve quality. Providing adequate funding to support these minimum staffing levels and targeting the funding to ensure that the funds are used for direct-care staff are essential elements of any legislation to that effect. The US literature has identified a minimum benchmark of 4.1 nursing hours per resident day, below which residents are more likely to experience harmful effects such as pressure ulcers and unexplained weight loss. Research on the generalizability of this benchmark to the Canadian context is urgently needed.
The residential care population is one of the most vulnerable in our society, and the residents and their families have little voice. Facilities caring for this population need to be licensed and adequately regulated. There should be regular unannounced inspections by trained inspectors and good information systems for reporting on quality measures. Families and residents should also be invited to complete anonymous surveys at regular intervals, and such a process should be a mandatory part of facility licensing.
Up-to-date information on direct-care staffing levels, inspection reports, consumer complaints and resident/family survey results should also be publicly available. This would be an important step toward balancing the information asymmetry in this sector. Although it is not a guarantee of quality, providing the public access to data on agreed-upon measures may encourage greater accountability on the part of facilities and governments.
Other policies to improve residential long-term care include developing broader networks of nonprofit facilities, fostering strong team leadership among staff, developing quality improvement programs to support good care, improving the alignment of the acute and residential care sectors, linking academic medical programs with the residential long-term care sector and providing high-quality end-of-life care to the residential care population.
Taking care of seniors at a time in their life when they are most vulnerable and need the most support or assistance may be one of the most important public policy challenges facing us over the next 30 years. The decisions we make about how to finance and deliver long-term care services will be crucial in ensuring that vulnerable seniors receive the quality of care they deserve.
Aaronson, W.E., J.S. Zinn, and M.D. Rosko. 1994. “Do For-Profit and Not-For-Profit Nursing Homes Behave Differently?” Gerontologist 34 (6): 775-86.
Ackermann, R.J., and K.A. Kemle. 1998. “The Effect of a Physician Assistant on the Hospitalization of Nursing Home Residents.” Journal of the American Geriatrics Society 46 (5): 610-14.
“Alberta Bonds Could Be Used to Build Group Homes, Long-Term Care Centres.” 2009. Toronto: Canadian Press.
Allen, P.D., W.C. Klein, and C. Gruman. 2003. “Correlates of Complaints Made to the Connecticut Long-Term Care Ombudsman Program.” Research on Aging 25 (6): 631-54.
Allman, R.M., C.A. Laprade, L.B. Noel, J.M. Walker, C.A. Moorer, M.R. Dear, and C.R. Smith. 1986. “Pressure Sores among Hospitalized Patients.” Annals of Internal Medicine 105 (3): 337-42.
American Medical Association. 1986. “Quality of Care – Council on Medical Service.” Journal of the American Medical Association 256 (8): 1032-4.
Amirkhanyan, A. 2008. “Privatizing Public Nursing Homes: Examining the Effects on Quality and Access.” Public Administration Review 68 (4): 665-80.
Anderson, G.L., M. Limacher, A.R. Assaf, T. Bassford, S.A. Beresford, H. Black, D. Bonds, R. Brunner, R. Brzyski, B. Caan, R. Chlebowski, D. Curb, M. Gass, J. Hays, G. Heiss, S. Hendrix, B.V. Howard, J. Hsia, A. Hubbell, R. Jackson, K.C. Johnson, H. Judd, J.M. Kotchen, L. Kuller, A.Z. LaCroix, D. Lane, R.D. Langer, N. Lasser, C.E. Lewis, J. Manson, K. Margolis, J. Ockene, M.J. O’Sullivan, L. Phillips, R.L. Prentice, C. Ritenbaugh, J. Robbins, J.E. Rossouw, G. Sarto, M.L. Stefanick, H.L. Van, J. Wactawski-Wende, R. Wallace, and S. Wassertheil-Smoller. 2004. “Effects of Conjugated Equine Estrogen in Postmenopausal Women with Hysterectomy: The Women’s Health Initiative Randomized Controlled Trial.” Journal of the American Medical Association 291 (14): 1701-12.
Anderson, R.A., K.N. Corazzini, and R.R. McDaniel, Jr. 2004. “Complexity Science and the Dynamics of Climate and Communication: Reducing Nursing Home Turnover.” Gerontologist 44 (3): 378-88.
Arling, G., T. Lewis, R.L. Kane, C. Mueller, and S. Flood. 2007. “Improving Quality Assessment through Multilevel Modeling: The Case of Nursing Home Compare.” Health Services Research 42 (3, part 1): 1177-99.
Armstrong, P., and T. Daly. 2004. “There Are Not Enough Hands: Conditions in Ontario’s Long-Term Care Facilities.” Canadian Union of Public Employees. Accessed September 2, 2010. https://cupe.ca/updir/CUPELTC-ReportEng1.pdf
Banaszak-Holl, J., W.B. Berta, D.M. Bowman, J.A.C. Baum, and W. Mitchell. 2002. “The Rise of Human Service Chains: Antecedents to Acquisitions and Their Effects on the Quality of Care in US Nursing Homes.” Managerial and Decision Economics 23 (4-5): 261-82.
Barry, T.T., D. Brannon, and V. Mor. 2005. “Nurse Aide Empowerment Strategies and Staff Stability: Effects on Nursing Home Resident Outcomes.” Gerontologist 45 (3): 309-17.
Bates-Jensen, B.M., J.F. Schnelle, C.A. Alessi, N.R. Al-Samarrai, and L. Levy-Storms. 2004. “The Effects of Staffing on In-Bed Times of Nursing Home Residents.” Journal of the American Geriatric Society 52 (6): 931-8.
Baumbusch, J.L. 2008. “Decomissioning Citizenship: The Organization of Long-Term Residential Care.” Unpublished doctoral thesis, University of British Columbia.
BCMA (see British Columbia Medical Association)
Bell, E. 2010. Research for Health Policy. New York: Oxford University Press.
Berta, W., A. Laporte, and V. Valdmanis. 2005. “Observations on Institutional Long-Term Care in Ontario: 1996-2002.” Canadian Journal on Aging 24 (1): 71-84.
Bostick, J.E., M.J. Rantz, M.K. Flesner, and C.J. Riggs 2006. “Systematic Review of Studies of Staffing and Quality in Nursing Homes.” Journal of the American Medical Directors Association 7 (7): 366-76.
Bowblis, J.R. 2009. “Ownership Conversion by Nursing Homes and the Quality of Care.” Miami University Farmer School of Business Department of Economics Working Paper 2009-10. Accessed July 31, 2010. https://www.fsb.muohio.edu/fsb/ecopapers/docs/bowblijr-2009-10-paper.pdf
Boyne, G.A. 2003. “Sources of Public Service Improvement: A Critical Review and Research Agenda.” Journal of Public Administration Research and Theory 13 (3): 367-94.
Bravo, G., P. De Wals, M.F. Dubois, and M. Charpentier. 1999a. “Correlates of Care Quality in Long-Term Care Facilities: A Multilevel Analysis.” Journals of Gerontology: Psychological Sciences and Social Sciences 54B (3): P180-8.
Bravo, G., M.F. Dubois, M. Charpentier, P. De Wals, and A. Emond. 1999b. “Quality of Care in Unlicensed Homes for the Aged in the Eastern Townships of Quebec.” Canadian Medical Association Journal 160 (10): 1441-5.
Bravo, G., M.F. Dubois, P. De Wals, R. Hebert, and L. Messier. 2002. “Relationship between Regulatory Status, Quality of Care, and Three-Year Mortality in Canadian Residential Care Facilities: A Longitudinal Study.” Health Services Research 37 (5): 1181-96.
British Columbia. 2009. Community Care and Assisted Living Act, Residential Care Regulation [includes amendments up to B.C. Reg. 10/2010, January 15, 2010]. Victoria: Government of British Columbia. Accessed July 31, 2010. https://www.bclaws.ca/EPLibraries/bclaws_new/document/
ID/freeside/96_2009#section26
British Columbia Medical Association (BCMA). 2008. Bridging the Islands: Rebuilding BC’s Home and Community Care System. Vancouver: BCMA. Accessed July 31, 2010. https://www.bcma.org/files/HCC_paper.pdf
Britton, M. 2002. “The Epidemiology of Mesothelioma.” Seminars in Oncology 29 (1): 18-25.
Broemeling, A.M., M.J. McGregor, J. Kozak, K.M. McGrail, L.A. Ronald, Y. Araki, and J. Murphy. 2010. Predictors ofHospitalization among Long-Term Home Health Services Clients in One Regional Health Authority in BC: What the Interrai-HC Data Tell Us. Kelowna, BC: Interior Health Authority.
Canadian Healthcare Association (CHA). 2009. New Directions for Facility-Based Long Term Care. Ottawa: CHA. Accessed July 31, 2010. https://www.cha.ca/index.php?option=com_
content&view=article&id=223&Itemid=101
Canadian Institute for Health Information (CIHI). 2005. Exploring the 70/30 Split: How Canada’s Health Care System Is Financed. Ottawa: CIHI. Accessed July 31, 2010. https://secure.cihi.ca/ cihiweb/dispPage.jsp?cw_page=AR_1282_E
—————–. “Health Expenditures by Year.” 2009. Ottawa: CIHI.
Canadian Union of Public Employees (CUPE). 2009. Residential Long-Term Care in Canada: Our Vision for Better Seniors Care. Ottawa: CUPE. Accessed July 31, 2010. https://cupe.ca/
elderly/report-seniors-care-crisis
Carter, K.S. 2009. The Best of Care: Getting It Right for Seniors in British Columbia: Part 1. Victoria: BC Ombudsperson. Accessed July 31, 2010. https://www.ombudsman.bc.ca/ images/resources/reports/Public_Reports/Public_Report_
No_46.pdf
Carter, M.W. 2003. “Factors Associated with Ambulatory Care-Sensitive Hospitalizations among Nursing Home Residents.” Journal on Aging and Health 15 (2): 295-331.
Castle, N.G. 2000a. “Deficiency Citations for Physical Restraint Use in Nursing Homes.” Journals of Gerontology: Psychological Sciences and Social Sciences 55B (1): S33-40.
—————–. 2000b. “Differences in Nursing Homes with Increasing and Decreasing Use of Physical Restraints.” Medical Care 38 (12): 1154-63.
—————–. 2009. “Nursing Home Caregiver Staffing Levels and Quality of Care: A Literature Review.” Journal of Applied Gerontology 27 (4): 375-405.
Castle, N.G., and J. Engberg. 2005. “Staff Turnover and Quality of Care in Nursing Homes.” Medical Care 43 (6): 616-26.
—————–. 2007. “The Influence of Staffing Characteristics on Quality of Care in Nursing Homes.” Health Services Research 42 (5): 1822-47.
Castle, N.G., and B. Fogel. 1998. “Characteristics of Nursing Homes That Are Restraint Free.” Gerontologist 38 (2): 181-8.
Castle, N.G., and S. Myers. 2006. “Mental Health Care Deficiency Citations in Nursing Homes and Caregiver Staffing.” Administration and Policy in Mental Health and Mental Health Services Research 33 (2): 215-25.
Castonguay, C., J. Marcotte, and M. Venne. 2008. En avoir pour notre argent: Rapport du Groupe de Travail sur le Financement du Système de Santé. Quebec: Government of Quebec.
CBC News. 2009. “”˜Horror Stories’ from Ontario Nursing Homes Worry Ombudsman.” Accessed July 31, 2010. https://www.cbc.ca/canada/toronto/story/2008/07/03/
nursing-homes.html
Centers for Medicare and Medicaid Services (CMS). 2001. Report to Congress: Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes: Phase II Final Report. Baltimore: CMS. Accessed July 31, 2010. https://www.allhealth.org/briefingmaterials/abt-nursestaffingratios%2812-01%29-999.pdf
Centre for Reviews and Dissemination (CRD). 2008. Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. York, UK: University of York. Accessed July 31, 2010. https://www.york.ac.uk/inst/crd/systematic_reviews_book.htm
CHA (see Canadian Healthcare Association)
CIHI (see Canadian Institute for Health Information)
Cleveland, G., B. Forer, D. Hyatt, C. Japel, and M. Krashinsky. 2008. “New Evidence about Child Care in Canada: Use Patterns, Affordability and Quality.” IRPP Choices 14 (12).
CMS (see Centers for Medicare and Medicaid Services)
Cohen, M., J. Murphy, K. Nutland, and A. Ostry. 2005. Continuing Care Renewal or Retreat? BC Residential and Home Health Care Restructuring, 2001-2004. Ottawa: Canadian Centre for Policy Alternatives. Accessed July 31, 2010. https://www.policyalternatives.ca/publications/reports/
continuing-care-renewal-or-retreat
Cohen, M., J. Tate, and J. Baumbusch. 2009. An Uncertain Future for Seniors: BC’s Restructuring of Home and Community Health Care, 2001-2008. Ottawa: Canadian Centre for Policy Alternatives. Accessed July 31, 2010. https://www.policyalternatives.ca/publications/reports/uncertain-future-seniors
Collier, E., and C. Harrington. 2008. “Staffing Characteristics, Turnover Rates, and Quality of Resident Care in Nursing Facilities.” Research in Gerontological Nursing 1 (3): 157-70.
Comondore, V.R., P.J. Devereaux, Q. Zhou, S.B. Stone, J.W. Busse, N.C. Ravindran, K.E. Burns, T. Haines, B. Stringer, D.J. Cook, S.D. Walter, T. Sullivan, O. Berwanger, M. Bhandari, S. Banglawala, J.N. Lavis, B. Petrisor, H. Schunemann, K. Walsh, N. Bhatnagar, and G.H. Guyatt. 2009. “Quality of Care in For-Profit and Not-for-Profit Nursing Homes: Systematic Review and Meta-analysis.” British Medical Journal 339:b2732.
CUPE (see Canadian Union of Public Employees)
Davis, M.A. 1993. “Nursing Home Ownership Revisited: Market, Cost and Quality Relationships.” Medical Care 31 (11): 1062-8.
Delgado-Rodriguez, M., and J. Llorca. 2004. “Bias.” Journal of Epidemiology and Community Health58 (8): 635-41.
Devereaux, P.J., P.T. Choi, C. Lacchetti, B. Weaver, H.J. Schunemann, T. Haines, J.N. Lavis, B.J. Grant, D.R. Haslam, M. Bhandari, T. Sullivan, D.J. Cook, S.D. Walter, M. Meade, H. Khan, N. Bhatnagar, and G.H. Guyatt. 2002a. “A Systematic Review and Meta-analysis of Studies Comparing Mortality Rates of Private For-Profit and Private Not-for-Profit Hospitals.” Canadian Medical Association Journal 166 (11): 1399-406.
Devereaux, P.J., H.J. Schunemann, N. Ravindran, M. Bhandari, A.X. Garg, P.T. Choi, B.J. Grant, T. Haines, C. Lacchetti, B. Weaver, J.N. Lavis, D.J. Cook, D.R. Haslam, T. Sullivan, and G.H. Guyatt. 2002b. “Comparison of Mortality between Private For-Profit and Private Not-for-Profit Hemodialysis Centers: A Systematic Review and Meta-analysis.” Journal of the American Medical Association 288 (19): 2449-57.
Donabedian, A. 1966. “Evaluating the Quality of Medical Care.” Milbank Memorial Fund Quarterly 44 (3): 166-206.
Doupe, M., M. Brownell, A. Kozyrskyj, N. Dik, C. Burchill, M. Dahl, D. Chateau, C. De Coster, A. Hinds, and J. Bodnarchuk. 2006. Using Administrative Data to Develop Indicators of Quality Care in Personal Care Homes. Winnipeg: Manitoba Centre for Health Policy, University of Manitoba. Accessed July 31, 2010. https://mchp-appserv.cpe.umanitoba.ca/reference/pch.qi.pdf
Engle, V.F. 1998. “Care of the Living, Care of the Dying: Reconceptualizing Nursing Home Care.” Journal of the American Geriatric Society 46 (9): 1172-4.
Ernst and Young Orenda. 2006. “Étude sur les PPP canadiens: Les défis du marché canadien des PPP.” Accessed October 18, 2010. https://www.ppp.gouv.qc.ca/admin/Fichiers/ Rapport%20lies%20d%C3%A9fisdumarch%C3%A9
canadien%20PPPCDN_P3_FR.pdf
Fried, T.R., M.R. Gillick, and L.A. Lipsitz. 1997. “Short-Term Functional Outcomes of Long-Term Care Residents with Pneumonia Treated with and without Hospital Transfer.” Journal of the American Geriatric Society 45 (3): 302-6.
Frohlich, N., C. De Coster, and N. Dik. 2006. Estimating Personal Care Home Bed Requirements. Winnipeg: Manitoba Centre for Health Policy, University of Manitoba. Accessed July 31, 2010. https://umanitoba.ca/centres/mchp/reports01-03.htm
Gagné, R., P. Meekison, J. Gross Stein, and L. Murray. 2006. Reconciling the Irreconcilable: Addressing Canada’s Fiscal Imbalance. Ottawa: Council of the Federation. Accessed July 31, 2010. https://www.councilofthefederation.ca/pdfs/ Report_Fiscalim_Mar3106.pdf
Gamble, J. 2010. “Lung Cancer and Diesel Exhaust: A Critical Review of the Occupational Epidemiology Literature.” Critical Reviews in Toxicology 40 (3): 189-244.
Gillick, M.R., N.A. Serrell, and L.S. Gillick. 1982. “Adverse Consequences of Hospitalization in the Elderly.” Social Science and Medicine 16 (10): 1033-8.
Glouberman S., J. Richards, M.E. Bestawi, R. Seidman-Carlson, and L. Teperman. 2007. “Reconnecting to Care: A Nursing Initiative at the Baycrest Geriatric Health System.” Nursing Leadership 20 (2).
Gordis, L. 2009. Epidemiology. Philadelphia: Saunders Elsevier.
Grabowski, D.C. 2005. “Consumer Complaints and Nursing Home Quality.” Medical Care 43 (2): 99-101.
Grabowski, D.C., and J.J. Angelelli. 2004. “The Relationship of Medicaid Payment Rates, Bed Constraint Policies, and Risk-Adjusted Pressure Ulcers.” Health Services Research 39 (4, part 1): 793-812.
Grabowski, D.C., and N.G. Castle. 2004. “Nursing Homes with Persistent High and Low Quality.” Medical Care Research and Review 61 (1): 89-115.
Grabowski, D.C., and R.A. Hirth. 2003. “Competitive Spillovers across Non-profit and For-Profit Nursing Homes.” Journal of Health Economics 22 (1): 1-22.
Grabowski, D.C., and D.G. Stevenson. 2008. “Ownership Conversions and Nursing Home Performance.” Health Services Research 43 (4): 1184-2003.
Grabowski, D.C., K.A. Stewart, S.M. Broderick, and L.A. Coots. 2008. “Predictors of Nursing Home Hospitalization: A Review of the Literature.” Medical Care Research”‚and Review 65 (1): 3-39.
Gray, B.H., and W.J. McNerney. 1986. “For-Profit Enterprise in Health Care. The Institute of Medicine Study.” New England Journal of Medicine 314 (23): 1523-8.
Guyatt, G.H., A.D. Oxman, G.E. Vist, R. Kunz, Y. Falck-Ytter, P. Alonso-Coello, and H.J. Schunemann. 2008. “GRADE: An Emerging Consensus on Rating Quality of Evidence and Strength of Recommendations.” British Medical Journal 336 (7650): 924-6.
Harchaoui, T.M, F. Tarkhani, and P. Warren. 2003. “Public Infrastructure in Canada:Where Do We Stand?”Insights on the Canadian Economy, Statistics Canada, November.
Harrington, C. 2001. “Regulating Nursing Homes: Residential Nursing Facilities in the United States.” British Medical Journal 323 (7311): 507-10.
—————–. 2008. “Public vs. Private Nursing Homes: Lessons from the US.” Paper presented at the public forum “Who Is Minding the Store? The Privatization of Long-Term Care and What It Means for Care Quality.” Canadian Doctors for Medicare, BC Health Coalition, and BC Association of Geriatric Care Physicians, November 5, 2008.
Harrington C., H. Carillo, B.W. Blank, and T. O’Brian. 2010a. “Nursing Facilities, Staffing, Residents and Facility Deficiencies, 2004 Through 2009.” University of California, San Francisco. Accessed December 31, 2010. https://www.theconsumervoice.org/sites/default/files/
advocate/action-center/OSCAR-2010.pdf ink
Harrington, C., C. Hauser, B. Olney, P.V. Rosenau, and H. Carrillo. 2010b. “Organizational Structure, Financing, and Quality of the Ten Largest For-Profit Nursing Home Chains in the US.” Unpublished paper.
Harrington, C., J. O’Meara, E. Collier, T. Kang, C. Stephens, and J. Zhang J. 2010c. Impact of California’s Medi-Cal Long Term Care Reimbursement Act on Access, Quality, and Costs. San Francisco: Center for Personal Assistance Services, University of California, San Francisco. Accessed July 31, 2010. https://www.pascenter.org/publications/ publication_home.php?id=828&focus=PAS
Harrington, C., J. O’Meara, M. Kitchener, L.P. Simon, and J.F. Schnelle. 2003. “Designing a Report Card for Nursing Facilities: What Information Is Needed and Why.” Special issue, Gerontologist 43 (2): 47-57.
Harrington, C., and J.H. Swan. 2003. “Nursing Home Staffing, Turnover, and Case Mix.” Medical Care Research and Review 60 (3): 366-92.
Harrington, C., J.H. Swan, and H. Carrillo. 2007. “Nurse Staffing Levels and Medicaid Reimbursement Rates in Nursing Facilities.” Health Services Research 42 (3, part 1): 1105-29.
Harrington, C., T. Tsoukalas, C. Rudder, R.J. Mollot, and H. Carrillo. 2008. “Variation in the Use of Federal and State Civil Money Penalties for Nursing Homes.” Gerontologist 48 (5): 679-91.
Harrington, C., S. Woolhandler, J. Mullan, H. Carrillo, and D.U. Himmelstein. 2001. “Does Investor Ownership of Nursing Homes Compromise the Quality of Care?” American Journal of Public Health 91 (9): 1452-5.
Harrington, C., C. Kovner, M. Mezey, J. Kayser-Jones, S. Burger, M. Mohler, R. Burke, and D. Zimmerman. 2000a. “Experts Recommend Minimum Nurse Staffing Standards for Nursing Facilities in the United States.” Gerontologist 40 (1): 5-16.
Harrington, C., D. Zimmerman, S.L. Karon, J. Robinson, and P. Beutel. 2000b. “Nursing Home Staffing and Its Relationship to Deficiencies.” Journals of Gerontology: Psychological Sciences and Social Sciences 55B (5): S278-87.
Health Canada. 2002. “Canada’s Aging Population.” Ottawa: Public Health Agency of Canada. Accessed July 31, 2010. https://www.phac-aspc.gc.ca/seniors-aines/alt-formats/ pdf/publications/public/various-variee/papier-fed-paper/
fedpager_e.pdf
Hill, A.B. 1965. “The Environment and Disease: Association and Causation.” Proceedings of the Royal Society of Medicine 58:295-300.
Hillmer, M.P., W.P. Wodchis, S.S. Gill, G.M. Anderson, and P.A. Rochon. 2005. “Nursing Home Profit Status and Quality of Care: Is There Any Evidence of an Association?” Medical Care Research and Review 62 (2): 139-66.
Himmelstein, D.U., S. Woolhandler, I. Hellander, and S.M. Wolfe. 1999. “Quality of Care in Investor-Owned vs Not-for-Profit HMOs.” Journal of the American Medical Association 282 (2): 159-63.
Hirdes, J.P., B.E. Fries, J.N. Morris, N. Ikegami, D. Zimmerman, D.M. Dalby, P. Aliaga, S. Hammer, and R. Jones. 2004. “Home Care Quality Indicators (HCQIs) Based on the MDS-HC.” Gerontologist 44 (5): 665-79.
Hirth, R.A., J. Banaszak-Holl, B.E. Fries, and M.E. Turenne. 2009. “Does Quality Influence Consumer Choice of Nursing Homes? Evidence from Nursing Home to Nursing Home Transfers.” Inquiry – Excellus Health Plan ABI/Inform global 40 (4): 343-61.
Hollander, M.J., and E. Walker. 2010. Report on Continuing Care Organization and Terminology. Prepared on behalf of the Federal/Provincial/Territorial Committee of Officials (Seniors) for the Minister Responsible for Seniors. Ottawa: Public Health Agency of Canada. Accessed July 31, 2010. https://www.phac-aspc.gc.ca/seniors-aines/publications/pro/ caregiving-soins/care-soin/index-eng.php#toc
Horn, S.D., P. Buerhaus, N. Bergstrom, and R.J. Smout. 2005. “RN Staffing Time and Outcomes of Long-Stay Nursing Home Residents: Pressure Ulcers and Other Adverse Outcomes Are Less Likely as RNs Spend More Time on Direct Patient Care.” American Journal of Nursing 105 (11): 58-70.
Hughes, C.M., K.L. Lapane, and V. Mor. 2000. “Influence of Facility Characteristics on Use of Antipsychotic Medications in Nursing Homes.” Medical Care 38 (12): 1164-73.
Iacobacci, M. 2010. “Détruire les mythes: Une évaluation canadienne des partenariats public-privé pour les investissements en infrastructures.”Conference Board of Canada Report. Accessed October 28, 2010. https://www.conferenceboard. ca/documents.aspx?did=3432
IMF (see International Monetary Fund)
Infrastructure Ontario. 2010. “Non-profit Long-term Care Homes.” Accessed November 9, 2010. https://www.infrastructureontario.ca/en/loan/long_term_care/index.asp
Institute for Healthcare Improvement (IHI). 2010. “Extend the Chain”: Work with Resources Outside of the Hospital to Improve the Flow of Care. Cambridge, MA: IHI. Accessed July 31, 2010. https://www.ihi.org/IHI/Topics/Flow/ PatientFlow/Changes/Extend+the+ChainWorkwithResourcesOutsideoftheHospitaltoImprovetheFlowofCare.htm
International Monetary Fund (IMF). 2004. Public-Private Partnerships. Washington: Fiscal Affairs Department, IMF. Accessed July 31, 2010. https://www.imf.org/external/np/ fad/2004/pifp/eng/031204.pdf
–––. 2009. World Economic Crisis: IMF Urges G-20 States to Take More Decisive Action to Combat Crisis. Washington: IMF. Accessed July 31, 2010. https://www.imf.org/external/pubs/ ft/survey/so/2009/new020509a.htm
Intrator, O., N.G. Castle, and V. Mor. 1999. “Facility Characteristics Associated with Hospitalization of Nursing Home Residents: Results of a National Study.” Medical Care 37 (3): 228-37.
Japel, C., R.A. Tremblay, and S. Côté. 2005. “Quality Counts!” IRPP Choices 11 (5).
Kane, R.A., K.C. Kling, B. Bershadsky, R.L. Kane, K. Giles, H.B. Degenholtz, J. Liu, and L.J. Cutler. 2003. “Quality of Life Measures for Nursing Home Residents.” Journals of Gerontology: Psychological Sciences and Social Sciences 58B (3): 240-8.
Kane, R.L., R. Bell, S. Riegler, A. Wilson, and R.A. Kane. 1983. “Assessing the Outcomes of Nursing-Home Patients.” Journal of Gerontology 38 (4): 385-93.
Kayser-Jones, J. 1996. “Mealtime in Nursing Homes: The Importance of Individualized Care.” Journal of Gerontological Nursing 22 (3): 26-31.
—————–. 1997. “Inadequate Staffing at Mealtime: Implications for Nursing and Health Policy.” Journal of Gerontological Nursing 23 (8): 14-21.
Kerrison, S.H., and A.M. Pollock. 2001. “Caring for Older People in the Private Sector in England.” British Medical Journal 323 (7312): 566-9.
Kim, H., C. Harrington, and W.H. Green. 2009. “Registered Nurse Staffing Mix and Quality of Care in Nursing Homes: A Longitudinal Analysis.” Gerontologist 49 (1): 81-90.
Kirkevold, H. 2008. “The Norwegian Teaching Home Program: Developing a Model for Systematic Practice Development in the Nursing Home Sector.” International Journal of Older People Nursing 3 (4): 282-6.
Konetzka, R.T. 2009. “Do Not-for-Profit Nursing Homes Provide Better Quality?” British Medical Journal 339:b2683.
Konetzka, R.T., W. Spector, and T. Shaffer. 2004. “Effects of Nursing Home Ownership Type and Resident Payer Source on Hospitalization for Suspected Pneumonia.” Medical Care 42 (10): 1001-8.
Konetzka, R.T., S.C. Stearns, and J. Park. 2008. “The Staffing-Outcomes Relationship in Nursing Homes.” Health Services Research 43 (3): 1025-42.
Konetzka, R.T., D. Yi, E.C. Norton, and K.E. Kilpatrick. 2004. “Effects of Medicare Payment Changes on Nursing Home Staffing and Deficiencies.” Health Services Research 39 (3): 463-88.
Kramer, A.M., and R. Fish. 2001. “The Relationship between Nurse Staffing Levels and the Quality of Nursing Home Care.” In Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes: Phase II Final Report. Baltimore: Centers for Medicare and Medicaid Services (CMS). Accessed July 31, 2010. https://www.cms.hhs.gov/medicaid/reports/ rp1201home.asp
Lawlor, D.A., S.G. Davey, and S. Ebrahim. 2004. “Commentary: The Hormone Replacement-Coronary Heart Disease Conundrum: Is This the Death of Observational Epidemiology?” International Journal”‚of Epidemiology 33 (3): 464-7.
Lee, C.L., T.L. Liu, L.J. Wu, U.L. Chung, and C.L. Lee. 2002. “Cost and Care Quality between Licensed Nursing Homes under Different Types of Ownership.” Journal of Nursing Research 10 (2): 151-9.
Levine, D. 2005. “A Healthcare Revolution: Quebec’s New Model of Healthcare.” Healthcare Quarterly 8 (4): 37-42.
Liberati, A., D.G. Altman, J. Tetzlaff, C. Mulrow, P.C. Gotzsche, J.P. Ioannidis, M. Clarke, P.J. Devereaux, J. Kleijnen, and D. Moher. 2009. “The PRISMA Statement for Reporting Systematic Reviews and Meta-analyses of Studies That Evaluate Healthcare Interventions: Explanation and Elaboration.” British Medical Journal 339:b2700.
Mackenzie, H. 2004. Financing Canada’s Hospitals: Public Alternatives to P3s. Toronto: Ontario Health Coalition.
McGrail, K.M., A.M. Broemeling, M. McGregor, K. Salomons, L.A. Ronald, and R. McKendry. 2008. Home Health Services in British Columbia: A Portrait of Users and Trends over Time. Vancouver: UBC Centre for Health Services and Policy Research, University of British Columbia. Accessed July 31, 2010. https://www.chspr.ubc.ca/files/publications/ 2008/chspr08-15.pdf
McGrail, K.M., M.J. McGregor, M. Cohen, R.B. Tate, and L.A. Ronald. 2007. “For-Profit versus Not-for-Profit Delivery of Long-Term Care.” Canadian Medical Association Journal 176 (1): 57-8.
McGrail, K.M, L. Meredith, M.J. McGregor, A.M. Broemeling, K. Salomons, S. Peterson, R. McEndry, and M. Barer. Forthcoming. “Who Uses Assisted Living in British Columbia? An Initial Exploration.” UBC Centre for Health Services and Policy Research, University of British Columbia.
McGregor, M.J., M. Cohen, K.M. McGrail, A.M. Broemeling, R.N. Adler, M. Schulzer, L. Ronald, Y. Cvitkovich, and M. Beck. 2005. “Staffing Levels in Not-for-Profit and For-Profit Long-Term Care Facilities: Does Type of Ownership Matter?” Canadian Medical Association Journal 172 (5): 645-9.
McGregor, M.J., R.B. Tate, K.M. McGrail. 2007. “Variation in Site of Death among Nursing Home Residents in British Columbia, Canada.” Journal of Palliative Medicine 10 (5): 1128-36.
McGregor, M.J., R.B. Tate, K.M. McGrail, L. Ronald, A.M. Broemeling, and H.J. Cohen. 2006. “Care Outcomes in Long-Term Care Facilities in British Columbia, Canada: Does Ownership Matter?” Medical Care 44 (10): 929-35.
McGregor M.J., J. Baumbush, R.B. Abu-Laban, K.M. McGrail, D. Andrusiek, J. Globerman, et al. 2010a. “A Survey of Nursing Home Organizational Characteristics Associated with Hospital Transfers and Care Quality in One Large British Columbia Health Region.” Unpublished paper.
McGregor, M.J., R.B. Tate, L.A. Ronald, K.M. McGrail, M.B. Cox, W. Berta, and A.M. Broemeling. 2010b. “Staffing in Long-Term Care in British Columbia, Canada: A Longitudinal Study of Differences by Facility Ownership, 1996-2006.” Health Reports 21 (4): 1-7.
Medicare. 2010. “Nursing Home Compare.” Baltimore: CMS. Accessed July 31, 2010. https://www.medicare.gov/ NHCompare/Include/DataSection/Questions/Proximity
Search.asp?bhcp=1
Mezey, M.D., E.L. Mitty, and S.G. Burger. 2008. “Rethinking Teaching Nursing Homes: Potential for Improving Long-Term Care.” Gerontologist 48 (1): 8-15.
Mor, V., K. Berg, J. Angelelli, D. Gifford, J. Morris, and T. Moore. 2003. “The Quality of Quality Measurement in U.S. Nursing Homes.” Special issue, Gerontologist 43 (2): 37-46.
Mor, V., O. Intrator, Z. Feng, and D.C. Grabowski. 2010. “The Revolving Door of Rehospitalization from Skilled Nursing Facilities.” Health Affairs 29 (1): 57-64.
Mukamel, D.B., and W.D. Spector. 2003. “Quality Report Cards and Nursing Home Quality.” Special issue, Gerontologist 43 (2): 58-66.
Murphy, J. 2006. Residential Care Quality: A Review of the Literature on Nurse Staffing and Quality of Care. Vancouver: Nursing Directorate, British Columbia Ministry of Health. Accessed July 31, 2010. https://www.heu.org/~DOCUMENTS/research_reports/November%202006%20CNAC%20report%20on%20residential%20care%20staffing%20and%20quality%20of%20care.pdf
O’Neill, C., C. Harrington, M. Kitchener, and D. Saliba. 2003. “Quality of Care in Nursing Homes: An Analysis of Relationships among Profit, Quality, and Ownership.” Medical Care 41 (12): 1318-30.
Ontario Ministry of Health and Long-Term Care (MOHLTC). 2009. “Seniors’ Care: Long-Term Care Homes.” Toronto: Government of Ontario. Accessed July 31, 2010. https://www.health.gov.on.ca/english/public/program/ltc/15_facilities.html
Park, J., and S.C. Stearns. 2009. “Effects of State Minimum Staffing Standards on Nursing Home Staffing and Quality of Care.” Health Services Research 44 (1): 56-78.
Pearson, A., S. Hocking, S. Mott, and A. Riggs. 1992. “Skills Mix in Australian Nursing Homes.” Journal of Advanced Nursing 17 (7): 767-76.
PriceWaterhouseCoopers. 2001. The PriceWaterhouseCoopers Report on Chronic and Long Term Care. Markham, ON: Ontario Long Term Care Association; Woodbridge, ON: Ontario Association of Non-profit Homes and Services for Seniors.
Quebec. 2009. “Ajout de 200 places d’hébergement et de soins de longue durée: Le gouvernement du Québec donne le coup d’envoi aux travaux de construction.” News release, April 24. Quebec: Government of Quebec. Accessed July 31, 2010. https://communiques.gouv.qc.ca/gouvqc/communiques/
GPQF/Avril2009/24/c4921.html
Ramage-Morin, P.L. 2006. “Successful Aging in Healthcare Institutions.” Health Reports 16:S47-56. Ottawa: Statistics Canada, Health Statistics Division.
Rantz, M.J., L. Hicks, V. Grando, G.F. Petroski, R.W. Madsen, D.R. Mehr, V. Conn, M. Zwygart-Staffacher, J. Scott, M. Flesner, J. Bostick, R. Porter, and M. Maas. 2004. “Nursing Home Quality, Cost, Staffing, and Staff Mix.” Gerontologist 44 (1): 24-38.
Rantz, M.J., A. Vogelsmeier, P. Manion, D. Minner, B. Markway, V. Conn, M.A. Aud, and D.R. Mehr. 2003. “Statewide Strategy to Improve Quality of Care in Nursing Facilities.” Gerontologist 43 (2): 248-58.
Rossouw, J.E., G.L. Anderson, R.L. Prentice, A.Z. LaCroix, C. Kooperberg, M.L. Stefanick, R.D. Jackson, S.A. Beresford, B.V. Howard, K.C. Johnson, J.M. Kotchen, and J. Ockene. 2002. “Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal Women: Principal Results from the Women’s Health Initiative Randomized Controlled Trial.” Journal of the American Medical Association 288 (3): 321-33.
Rothman, K.J., S. Greenland, and T.L. Lash. 2008. Modern Epidemiology. 3rd ed. Philadelphia: Lippincott-Williams-Wilkins.
Schnelle, J.F., M.P. Cadogan, J. Yoshii, N.R. Al-Samarrai, D. Osterweil, B.M. Bates-Jensen, and S.F. Simmons. 2003. “The Minimum Data Set Urinary Incontinence Quality Indicators: Do They Reflect Differences in Care Processes Related to Incontinence?” Medical Care 41 (8): 909-22.
Schnelle, J.F., S. Cretin, D. Saliba, and S.F. Simmons. 2001. “Minimum Nurse Aide Staffing Required to Implement Best Practice Care in Nursing Homes.” In Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes: Phase II Final Report. Baltimore: Centers for Medicare and Medicaid Services (CMS). Accessed July 31, 2010. https://www.cms.hhs.gov/medicaid/reports/rp1201home.asp
Schnelle, J.F., S.F. Simmons, C. Harrington, M. Cadogan, E. Garcia, and M. Bates-Jensen. 2004. “Relationship of Nursing Home Staffing to Quality of Care.” Health Services Research 39 (2): 225-50.
Schnelle, J.F., V.A. Sowell, B. Traughber, and T. Hu. 1988. “A Behavioral Analysis of the Labor Cost of Managing Continence and Incontinence in Nursing Home Patients.” Journal of Organizational Behavior Managment 9 (2): 137-53.
Shapiro, E., and R.B. Tate. 1995. “Monitoring the Outcomes of Quality of Care in Nursing Homes Using Administrative Data.” Canadian Journal of Aging 14 (4): 755-68.
Sharkey, S. 2008. People Caring for People: Impacting the Quality of Life and Care for Residents of Long-Term Care Homes. A Report of the Independent Review of Staffing and Care Standards for Long-Term Care Homes in Ontario. Toronto: Ministry of Health and Long-Term Care. Accessed July 31, 2010. https://www.health.gov.on.ca/english/public/pub/ministry_
reports/staff_care_standards/staff_care_standards.pdf
Spector, W.D., T.M. Selden, and J.W. Cohen. 1998. “The Impact of Ownership Type on Nursing Home Outcomes.” Health Economics 7 (7): 639-53.
Spector, W.D., and H.A. Takada. 1991. “Characteristics of Nursing Homes That Affect Resident Outcomes.” Journal on Aging and Health 3 (4): 427-54.
Staples, B.C., and C. Wodok. 2008. “SALT Brief on Continuing Care.” Seniors Action Liaison Team. Accessed September 2, 2010. https://www.continuingcarewatch.com/pdf/SALT% 20Brief%20on%20Continuing%20Care%202008%202.pdf
Statistics Canada. 2007. A Portrait of Seniors in Canada, 2006. Cat. no. 89-519-XIE. Ottawa: Statistics Canada. Accessed July 31, 2010. https://www.statcan.gc.ca/pub/89-519-x/89-519-x2006001-eng.htm
—————–. 2008a. “Income in Canada 2006.” Ottawa: Statistics Canada. Catalogue no. 75-202-x. Ottawa: Statistics Canada. Accessed November 8, 2010. https://www.statcan.gc.ca/pub/
75-202-x/75-202-x2006000-eng.pdf
—————–. 2008b.“Residential Care Facilities, by Ownership, Principal Characteristic of Predominant Group of Residents and Size of Facility, Canada, Provinces and Territories, Annual (Number).” 1984/1985 to 2007/2008. CANSIM table no. 107-5501, series 5200. Accessed September 2, 2010. https://cansim2.statcan.gc.ca/cgi-win/cnsmcgi.pgm?Lang=E&ArrayId=1075501&Array_Pick=1&RootDir=CII/&ResultTemplate=CII/CII___
—————–. 2008c. Residential Care Facilities, 2006/2007. Cat. no. 83-237-X. Ottawa: Statistics Canada. Accessed July 31, 2010. https://dsp-psd.pwgsc.gc.ca/collection_2008/statcan/83-237-X/83-237-XIE2009001.pdf
—————–. 2010a. “Estimates of Population, by Age Group and Sex for July 1, Canada, Provinces and Territories, Annual (Persons),” 2006. CANSIM table no. 051-0001, series 6210. Ottawa: Statistics Canada. Accessed July 31, 2010. https://cansim2.statcan.ca/cgi-win/CNSMCGI.PGM
–––. 2010b. “Residents on Books in Residential Care Facilities, by Age Group, Sex, Principal Characteristic of the Predominant Group of Residents and Size of Facility, Canada, Provinces and Territories, Annual (Number), 2006.” CANSIM table no. 107-5504, series 3250. Ottawa: Statistics Canada. Accessed July 31, 2010. https://cansim2.statcan.ca/cgi-win/CNSMCGI.PGM
Stevenson, D.G. 2005. “Nursing Home Consumer Complaints and Their Potential Role in Assessing Quality of Care.” Medical Care 43 (2): 102-11.
–––. 2006. “Nursing Home Consumer Complaints and Quality of Care: A National View.” Medical Care Research and Review 63 (3): 347-68.
Stocks-Rankin, C.R. 2008. “Who Cares about Ownership? A Policy Report on For-Profit, Not-for-Profit and Public Ownership in Ontario Long Term Care.” Master’s thesis, University of Edinburgh.
Strom, B.L. 2005. Pharmacoepidemiology. 4th ed. New York: John Wiley and Sons.
Such, C.L., C. Harrington, R. Dunah, and R.W. Maynard. 1996. “Know Your Financing Options.” Journal of Long-Term Care Administration 24 (1): 19-23.
TD Bank Financial Group. 2004. “Mind the Gap: Finding the Money to Upgrade Canada’s Aging Public Infrastructure.” TD Economics Special Report. Accessed October 18, 2010. https://www.td.com/economics/special/infra04.pdf
Thompson, R.S., N.K. Hall, and M. Szpiech. 1999. “Hospitalization and Mortality Rates for Nursing Home-Acquired Pneumonia.” Journal of Family Practice 48 (4): 291-3.
Trinkoff, A.M., M. Johantgen, C. Muntaner, and R. Le. 2005. “Staffing and Worker Injury in Nursing Homes.” American Journal of Public Health 95 (7): 1220-5.
Walshe, K. 2001. “Regulating U.S. Nursing Homes: Are We Learning from Experience?” Health Affairs 20 (6): 128-44.
Wasson, J. H., R. Benjamin, D. Johnson, L.G. Moor, and T. Mackenzie. Forthcoming. “Patients Use the Internet to Enter the Medical Home.” Journal of Ambulatory Care Management 34 (1): 1-9.
Weech-Maldonado, R., L. Meret-Hanke, M.C. Neff, and V. Mor. 2004. “Nurse Staffing Patterns and Quality of Care in Nursing Homes.” Health Care Management Review 29 (2): 107-16.
Wunderlich, G.S., and P.O. Kohler, eds. 2001. Improving the Quality of Long Term Care. Committee on Improving Quality in Long-Term Care, Division of Health Care Services, Institute of Medicine. Washington: National Academies Press.
Yassi, A., M. Cohen, Y. Cvitkovich, I.H. Park, P.A. Ratner, A.S. Ostry, J. Village, and N. Polla. 2004. “Factors Associated with Staff Injuries in Intermediate Care Facilities in British Columbia, Canada.” Nursing Research 53 (2): 87-98.
Zimmer, J.G., and W.J. Hall. 1997. “Nursing Home-Acquired Pneumonia: Avoiding the Hospital.” Journal of the American Geriatric Society 45 (3): 380-1.
Zimmerman, S., A.L. Gruber-Baldini, J.R. Hebel, P.D. Sloane, and J. Magaziner. 2002. “Nursing Home Facility Risk Factors for Infection and Hospitalization: Importance of Registered Nurse Turnover, Administration, and Social Factors.” Journal of the American Geriatric Society 50 (12): 1987-95.
Zinn, J., W. Spector, L. Hsieh, and D.B. Mukamel. 2005. “Do Trends in the Reporting of Quality Measures on the Nursing Home Compare Web Site Differ by Nursing Home Characteristics?” Gerontologist 45 (6): 720-30.
In this appendix we summarize the recommendations regarding changes to the funding and delivery of Canadian residential long-term care from five major reports published in 2008 and 2009. The Canadian Centre for Policy Alternatives (CCPA) published a report written by Cohen, Tate and Baumbusch (2009) on residential care in British Columbia entitled Continuing Care Renewal or Retreat? BC Residential and Home Health Care Restructuring, 2001-2004. The report from the Canadian Healthcare Association (CHA), entitled New Directions for Facility-Based Long Term Care, also came out in 2009. The Canadian Union of Public Employees (CUPE) report (2009) is entitled Residential LongTerm Care in Canada: Our Vision for Better Seniors Care. Kim Carter is the ombudsperson in British Columbia, and the report she presented to the BC Legislature is entitled The Best of Care: Getting It Right for Seniors in British Columbia: Part 1 (2009). Finally, the report of the Independent Review of Staffing and Care Standards for Long-Term Care Homes in Toronto, by Shirlee Sharkey, was presented to the Ontario Minister of Health and LongTerm Care in 2008.
The federal government must:
Create a provincial Web site with facility-level information on:
In their study, Margaret McGregor and Lisa Ronald conclude that the type of ownership of residential long-term care facilities for frail seniors is a determinant of the quality of care provided, suggesting, among other things, that the lower staffing levels in for-profit homes is a contributing factor to the inferior quality of care they provide.
In Ontario, the “envelope” funding system, which ensures money paid for care is in fact spent on care, and an extensive system of reporting, auditing, and inspection of all homes – regardless of their governance structure – establishes a minimum threshold for quality in care delivery. Certainly, variations in quality exist in Ontario. However, that variation is not easily bifurcated between for-profit and nonprofit homes. Just as there are poorer quality for-profit and high quality nonprofit homes, there are also excellent for-profit homes and struggling nonprofits, suggesting that factors other than ownership type may contribute to differences in quality.
McGregor and Ronald’s paper is provocative, but must be viewed in the context of an ongoing discussion. This continuing work must be inspired by two fundamental questions: 1) What more do we need to know about long-term care quality to shape the policy that drives improvement over the long term? and 2) What can and should we be doing now to change outcomes and the experience of residents in the short term, regardless of the governance structure of homes?
While ownership type may be one factor in the quality equation, we must understand the effect of other organizational features that may have an equally significant impact on the quality of residential long-term care. Research in the Canadian context that examines the impact of leadership, communication and teamwork as elements of organizational capacity, and their link to organizational performance, is in its early phase and must be expanded. Investigation of the impact on residential care quality of the size of multihome organizations, whether for-profit or nonprofit, and of the size of individual homes, may reveal valuable information. But examination of these structural characteristics and their relation to quality must not distract us from the immediate opportunity and current thirst of providers for quality improvement strategies that can be deployed in their environments. Managers and direct care staff in homes seek sector-specific training, practical tools and resources that would enhance their quality improvement efforts and ultimately improve residents’ experience.
McGregor and Ronald present several recommendations that extend the dialogue about the quality of care beyond the nonprofit versus for-profit debate. In that regard, Ontario may be viewed as a learning laboratory for strategies that shift the long-term care delivery culture to one intensely focused on quality. Responding to public demand for transparency and accountability and care providers’ interest in quality, two Ontario programs, Residents First and Long-Term Care Public Reporting, are positioned to have a profound impact on the long-term care industry.
Residents First is a five-year sector-designed initiative, funded by the Ontario Ministry of Health and Long-Term Care, that supports long-term care homes in providing an environment for their residents that enhances their quality of life, by means of customized training, tools and resources. The initiative facilitates comprehensive and lasting change by strengthening the homes’ capacity for quality improvement. Over three-quarters of Ontario’s long-term care homes, representing a balance of nonprofit and for-profit homes, have now voluntarily engaged in the initiative (www.residentsfirst.ca)
Long-Term Care Public Reporting was launched in Ontario in early 2010. Already over 130 homes are voluntarily reporting outcomes data on 6 individual-home-level indicators and over 30 province-level indicators, on a public access Web site (www.ohqc.ca). By the end of 2011, all Ontario homes will be reporting data on the Web site. Together, these two programs will help support nonprofit and for-profit organizations in long-term residential care as they move toward change.
McGregor and Ronald’s paper should continue to fuel Canadian-based research on variations in quality, research that can be used to inform policies to provide a solid structural framework for continued improvement. We must also support individual homes as they embark on their own quality improvement journey, so that every resident across the country can expect the best possible care, regardless of the ownership structure of the home.
This study was published as part of the Faces of Aging research program under the direction of Sarah Fortin. The manuscript was copy-edited by Mary Williams, proofreading was by Barbara Czanecki, editorial coordination was by Francesca Worrall, production was by Chantal Létourneau, art direction was by Schumacher Design and print- ing was by AGL Graphiques.
Margaret J. McGregor is a clinical associate professor with the Department of Family Practice and a research associate with the Centre for Health Services Policy Research at the University of British Columbia. She is also a research associate with the Vancouver Coastal Health Research Institute Centre for Clinical Epidemiology and Evaluation. She has completed a number of research projects in health services delivery, and she is supported in her research by a Community-based Clinician Investigator award, funded by the University of British Columbia Department of Family Practice Division of Geriatrics and the Centre for Health Services and Policy Research. She is also a family physician at the Mid-Main Community Health Centre in Vancouver, where part of her practice involves providing care to patients in residential long-term care.
Lisa A. Ronald is a researcher with the Family Practice Research Office at the Vancouver Coastal Health Research Institute’s Centre for Clinical Epidemiology and Evaluation. She holds MSc degrees from the University of British Columbia and the Liverpool School of Tropical Medicine, and is a PhD candidate in epidemiology at McGill University. She has worked on a number of research projects related to health services and aging.
To cite this document:
McGregor, Margaret J., and Lisa A. Ronald. 2011. Residential Long-Term Care for Canadian Seniors: Nonprofit, For- Profit or Does It Matter? IRPP Study, No. 14. Montreal: Institute for Research on Public Policy.
The IRPP is grateful to Health Canada, Human Resources and Skills Development Canada, the Public Health Agency of Canada, Canadian Institutes of Health Research, the governments of Alberta (Seniors and Community Support) and Québec (Ministère de la Santé et des Services sociaux), the Canadian Health Services Research Foundation, the BMO Financial Group, and GlaxoSmithKline for their financial support of the April 2-3, 2009, conference “When I’m 64…Defining Care-Giving Policy for an Aging Canada,” at which a preliminary version of this study was presented.
