
Les tendances démographiques associées au vieillissement de la population sont connues depuis des décennies, pourtant, le Canada n’a toujours pas défini une stratégie globale pour faire face aux répercussions socioéconomiques à long terme de ce phénomène, et moins encore à ses conséquences immédiates pour ce qui est des soins aux personnes âgées. Cette étude de Harvey Lazar part du triple constat d’un déséquilibre entre la demande et la disponi- bilité des soins, d’une éventuelle aggravation de ce déséquilibre et d’une nécessaire réévalua- tion du rôle du gouvernement fédéral à cet égard.
En matière de soins, la responsabilité constitutionnelle appartient aux gouvernements provin- ciaux et territoriaux, mais le gouvernement fédéral lui aussi joue un rôle important. En effet, bien que les provinces planifient, gèrent et supervisent la prestation des soins de santé et des services sociaux, les programmes fédéraux de pension et de sécurité du revenu pour personnes âgées et les paiements de transfert aux provinces ont une grande influence sur la disponibilité des soins et leur accessibilité. À l’heure du vieillissement démographique, d’une pénurie appréhendée de main-d’œuvre et de l’accentuation des pressions sur le système de santé, Ottawa sera vraisemblablement appelé à faire davantage.
Harvey Lazar examine donc le rôle actuel et les possibilités d’action du gouvernement fédéral au chapitre des soins aux personnes âgées. Il propose un éventail de mesures qui permettraient d’intervenir à la fois du côté de la demande et de l’offre, et qui seraient adaptées aux particu- larités du continuum de soins. Il évalue ensuite ces options afin de déterminer si elles sont conformes : 1) au partage constitutionnel des pouvoirs législatifs et au bon fonctionnement de la fédération ; 2) à 10 critères et objectifs de « bonne » politique publique dans ce domaine.
L’auteur en conclut qu’Ottawa dispose d’une marge de manœuvre appréciable pour répondre aux besoins grandissants des personnes âgées et au sous-financement des soins sans empiéter sur le leadership des provinces et territoires. Bon nombre des mesures qu’il propose visent directement les aînés pour les protéger entre autres contre le coût prohibitif de certains soins et renforcer leur capacité financière afin qu’ils puissent se procurer les services dont ils ont besoin. Il met aussi de l’avant quelques mesures qui devraient accroître la capacité de presta- tion de soins partout au pays.
La prochaine occasion de prendre d’importantes décisions sur la question se présentera lors de la renégociation en 2014 des transferts fédéraux en matière de santé et de programmes sociaux. Or il revient à Ottawa d’établir un diagnostic clair sur les besoins futurs de soins aux personnes âgées à l’échelle du pays. Il lui faudra également mieux définir son propre rôle, tout en tenant compte de l’incidence de ses interventions sur l’efficacité des programmes de soins provinciaux.
Preparing for an aging society has long been recognized as an important multidimensional challenge for Canada. The prospect of this demographic transformation has prompted much research on the potential economic and social implications for individuals and society and has raised major public policy issues. In the 1970s and early 1980s, the main focus of research was on the retirement income system.1 In the 1980s and 1990s, the effects of popula- tion aging on health care expenditures began to garner much attention. Both topics remain on the policy research agenda to this day, but a third theme has been added in recent years: the availability and cost of care for seniors.
Seniors’ care is not an easy topic to research, partly because it involves informal interactions, financial and otherwise, within the family. Researchers have nonetheless made significant inroads in understanding the needs of care recipients and the sources of caregiving, which include the immediate and extended family, friends and neighbours, as well as community organizations, institutions (nursing homes, assisted living and complex care residences) and governments. There remain important research and knowledge gaps, however. For example, there is little information on the actual availability of informal caregivers for disabled individ- uals (e.g., the proximity of children or the health status of spouses), and there is still much to learn about the interaction between the formal and informal care networks and systems and how they might be affected by the ongoing demographic trends.
The issues related to the care system reach far beyond the front-line actors. All Canadians, regardless of age, are potential care recipients and caregivers. Once they reach their adult years they need to prepare for the contingency of receiving (as seniors or even younger) or providing (to a parent, spouse or friend) care. Like pension policy, care policy affects relations among generations, and what is considered to be fair among generations will differ depending on whether it is assessed within the confines of the family or at the level of society.
The object of this study is to spur a public debate about one aspect of care policy that has received little attention to date.2 I am referring here to the way in which Canadian federalism affects the adequacy and availability of care for seniors. More particularly, I will look at the role the federal government has played in seniors’ care to date and what its options could be, and should be, as the population aging process unfolds.
The division of powers in our constitution and the lessons from seven decades of practical experience provide a general guide to the respective roles of federal and provincial/territorial governments in regard to seniors. Looking at the issue through this wide-angle lens, we see that the federal government has the lead role in providing pensions and other forms of income support, while the provinces plan, manage and oversee the delivery of health care and social services, including nonmedical care.
Since the current income support/service split between the two orders of government is relatively harmonious, it would be legitimate to ask whether it might not be best to leave well enough alone and not risk stirring up a hornet’s nest. The fact is that this broad description of “who does what” is far from perfect. Examples that do not fit within this neat division of tasks include provincial/territorial responsibility for social assistance and the federal government’s traditional role in the field of health care. It also brushes over the complex and inefficient overlap between the two orders of government in providing income support to people with disabilities.
This big picture also excludes the several ways in which the two jurisdictions inevitably inter- sect in carrying out their roles. At the constitutional level, provincial powers to make laws relating to old age and disability pensions trump federal authority. Accordingly, federal legisla- tion in these areas requires the acquiescence, if not the enthusiastic support, of the provinces. At the operational level, Ottawa’s decisions can influence provincial governments through either the level of income support that it provides to seniors or the magnitude of its cash transfers to the provinces and territories. Indeed, access to care for seniors is heavily affected by the decisions of both orders of government, as well as by the way in which governments interact.
Governments loom large in the lives of retired people. Over three-quarters of the aggregate income of those aged 65 and older comes from pensions — 42 percent from public pensions and 34 percent from private pensions. Lower-income Canadians are even more reliant on pub- lic plans, which account for as much as 80 to 100 percent of their income. The elderly also receive a larger proportion of the services they require through governments or government- subsidized activities than do people of working age.
The federal government delivers almost all public pensions (the main exception being the Quebec Pension Plan), and it also plays a large role in supporting private pension plans through income tax incentives. The federal government does not, of course, view its major retirement income programs (e.g., Old Age Security, Guaranteed Income Supplement, Canada Pension Plan, Registered Pension Plans and Registered Retirement Savings Plans) as part of the care system. But the impact of these policies on how care is organized is nonetheless pro- found. For example, the extent to which provincial/territorial governments need to plan for and subsidize care for an aging population is linked to the income levels of retired people. The more income they have, the more they are able to pay for services — including many kinds of care — on their own.
Another way that federal policies can influence provincial care decisions is through health and social transfers to the provinces. For instance, through the Canada Social Transfer (CST), Ottawa provides direct cash contributions to the provinces and territories, “notionally” (a term used by the federal Department of Finance) for social services, including care services. However, under current fiscal arrangements, the CST and other large federal transfers will expire on March 31, 2014. During the 2011 federal election campaign, the Conservative plat- form stated that the government “would work collaboratively with the provinces and territo- ries to renew the Health Accord” (Conservative Party 2011, 30), but it failed to mention the CST. Nor was the CST mentioned in the subsequent federal budget, presented on June 6, 2011.3 The reality is that the nonhealth costs of aging involve large sums and they interact sig- nificantly with the health costs.
Overall, the current relationship between the two orders of government in respect of pension policy and care challenges is low key, notwithstanding concerns about distressing system fail- ures in the recent past (such as the insolvency of some big private pension plans). For the most part, intergovernmental differences are managed without serious tensions. Indeed, there are ongoing discussions among federal, provincial and territorial governments on adding a further tranche to the retirement income system.4
This study is thus not motivated by a sense of crisis in intergovernmental relations. Rather, the main concern is that Canadians and their governments have not been preparing sufficiently for the kind of older society that they will constitute less than two decades from now. The aging of the population guarantees that the Canada of tomorrow will be quite different than the Canada of today. Since desirable policy out- comes on this front will likely require long lead times, postponing decisions about how to best prepare until some murky date in the future would in itself be a decision about the nature of that future.
Both orders of government now play a direct and/or indirect role in meeting care needs. The fact that their decision-making processes function largely independently of one another is far from a bad thing, since federal-provincial processes are not known for their speed or efficiency. Given their interaction on care issues, however, it is essential that each order of government understand not only the direct effects of its decisions on citizens, but also the consequences of these decisions for the programs of the other order of government in relation to these same cit- izens. The social issues are too important and the amounts of money too large for governments to ignore these ripple effects. These effects are not symmetrical. Provincial/territorial decisions only occasionally affect federal policies related to seniors’ well-being, whereas federal decisions have large, ongoing, direct and indirect impacts on provincial care programs. It is essential, therefore, that the federal government take into account how its interventions might influence the success of provincial care programs and ultimately the well-being of those who require care.
This study has two purposes. Assuming that Ottawa continues to respect the constitutional and policy pre-eminence of the provinces in care policy, the first is to determine whether and in what ways Canada’s federal structure influences the strategic choices available to the federal government in responding to the growing care needs of seniors. The second is to examine what Ottawa’s role could be in the future, and assess it in relation to two sets of standards: those that pertain to federalism principles and functional intergovernmental relations, and those that take account of other public policy criteria such as efficiency, equi- ty and accountability.
To foreshadow my conclusions: Notwithstanding constitutional limits on what the federal government can do directly in the sphere of caregiving, and taking full account of the leader- ship role of the provinces, there are many degrees of policy freedom available to Ottawa in addressing the growing and severely underfunded care needs of seniors.5 Viable options include measures aimed at seniors with light or intermediate care needs, as well as measures designed to enhance access to and provision of prolonged, complex care, and they relate to both the demand and the supply sides of caregiving.
Demand refers to the volume and the complexity of the care services required by seniors to ensure their well-being.6 Demand for care is determined by individuals’ health and personal cir- cumstances. Supply refers to all caregivers who are willing and able to perform the tasks for which there is a demand. These caregivers include family, friends, neighbours and volunteers who traditionally have not been paid for the assistance they provide (although this has begun to change); professional caregivers who work for provincial/territorial governments or nonprofit organizations; and businesses and individuals who provide care services at a price.
Demand is linked to the idea of personal autonomy. Ideally, personal autonomy means there are minimal limitations on a person’s activity and minimal restrictions on her participation in society.7 In the context of this study, it also entails having choices and the ability to make one’s own decisions in terms of caregivers and living conditions. In practice, however, care recipients’ personal autonomy will be determined by their health status and the formal and informal support systems and services that are available to them. Some of the measures required to maintain or increase care recipients’ personal autonomy may be costly, some may actually save money. In any event, personal autonomy is an issue that must be considered in any debate about care policy, and it is increasingly reflected in health officials’ efforts to enable people who require care to receive it at home for as long as possible.
Another important theme in this study is intergenerational equity. This refers to fairness in financial and other relationships between different generations. In one idealized version of this concept, each generation would pay for its own benefits, requiring no transfers from other generations. However, achieving a modicum of fairness between generations is very dif- ficult in practice. This becomes apparent as soon as one begins to consider the details of a new seniors’ care benefit: Should it be phased in over several decades, or should it be implemented immediately? If the phase-in period is long — say, 30 or 40 years — there will be little or no reduction in current unmet care needs. If the benefit is implemented fully without any phase- in, it may well be unfair to current taxpayers and, most acutely, to the younger cohorts. They may end up “paying twice,” contributing through higher taxes or other levies to cover the costs of the incremental care services made available to current seniors, and also paying for their own future benefits (by either participating in a public contributory plan or saving on their own). These younger taxpayers cannot rely on the future workforce to subsidize them when they become seniors, because with population aging, the future workforce may be too small and the future elderly too numerous to sustain the intergenerational subsidy. Balancing these intergenerational transfers in an aging society is a crucial issue in decision-making and a fundamental consideration in my analysis.8
These two themes can be linked. To the extent that maintaining seniors’ autonomy reduces public costs, it also reduces the size of any intergenerational transfers. When these considera- tions are aligned, policy is likely to be on a positive course. When they are in tension, policy choices are more difficult.
The study is organized as follows. In the first section, I set out six research premises regarding the care needs of seniors, the capacity of individuals to plan for themselves and Ottawa’s potential role in this policy area that frame the subsequent analysis. I also present the federalism/intergov- ernmental relations criteria and 10 other policy criteria that will be used to assess each option.
To provide a context for the discussion of care policy options that follows, I then review what Ottawa is currently doing, directly or indirectly, in relation to caregiving in four areas: income security for retirees, financing of social programs through the spending power, support for informal caregivers, and knowledge and information dissemination, and I examine how these various initiatives affect federal-provincial relations.
In the next two sections, I present a wide range of policy options available to the federal gov- ernment. The list of 19 options is not exhaustive, but it serves to illustrate the types of choices that could be considered. While some of the options are new, there is a precedent for most of them in current arrangements or post-Second World War history. A clear distinction is made in the analysis between the instruments that are suitable to address lighter and intermediate care needs and those that are more appropriate in the context of prolonged, complex care. Some options support the demand side of care, while others are meant to further develop the supply side. I then assess all of the options in terms of their probable effects on intergovern- mental relations and against the policy criteria referred to above.
It should be noted that the options are presented at a high level of generality, with little elaboration of design/costs and little reference to the current economic or fiscal environ- ment. The reasons for this are twofold. First, the purpose of this study is to explore the broad implications and trade-offs associated with different strategic directions, and more precisely to determine whether federalism will be a significant constraint on Ottawa’s strategic role going forward. Second, the time horizon for the issues examined in this study is years and even decades, not months. I conclude briefly in the final section.
The following premises frame the choice and assessment of possible options available to the federal government to support the provision of care for seniors.
First, the aging of the population will increase the need for care and the costs of care borne by governments. Like those of other industrialized countries, Canada’s population is aging, due to a persistently low birth rate and increasing life expectancy. The aging of the baby boom generation (those born between 1946 and 1965) adds a cohort-specific dimension to this situation (Schellenberg and Ostrovsky 2008). The first boomers turn 65 in 2011 and will reach 85 in 2031. At the same time, the working-age population is shrinking, and will continue to do so. Thus, beyond the increased demand for seniors’ care, the growth in the number of seniors relative to those of working age will lead to added pressure on provincial/territorial budgets.
But it is not just the growth in the number of elderly that will increase costs. There is also the fact that the demand for care is age related. A Statistics Canada study based on surveys conducted in 1994-95 and 2003 found that about 2.5 percent of those aged 18 and over received subsidized care, whereas the figure was around 20 percent for those aged 80 and over (Wilkins 2006, 39-42). With the aging of the population, current projections suggest that the number of elderly Canadians needing assistance will double in the next 30 years (Carrière et al. 2007, figure 6; Alzheimer Society 2010).
The unit costs of care services are also likely to increase, as the relative scarcity of caregivers will strengthen their bargaining position on wages and benefits. I use the word “likely,” because it is uncertain whether the labour market for caregivers behaves like a conventional service-industry market. If it does, wages will increase, and as compensation rises, the supply of caregivers will grow. If it does not, governments will need to consider supplementing care- givers’ compensation to increase their supply.
There are similar demographic concerns with informal care. Statistics Canada observes that “63 per cent of adults with disabilities who received help obtained it from members of their family living with them, 42 per cent received it from family members not living with them, 24 percent from friends and neighbours” (2003, 7). In 2007, 4.1 million Canadians aged 45 and over were providing some form of care to someone with a long-term health condition or physical limitation (Statistics Canada 2008a). However, socio-demographic trends suggest that the network of avail- able informal caregivers will be smaller in the future. And this, combined with greater demand for care, could lead to large and increasing shortfalls in informal caregivers going forward (Keefe, forthcoming). The magnitude of such shortfalls is difficult to project, but it is likely to be signifi- cant. The 2001 Participation and Activity Limitation Survey reported that roughly one-third of people with disabilities reported unmet care needs (Statistics Canada 2003, 7). Another survey found that while more people received subsidized home care in 2003 than in 1994-95, the pro- portion of people needing but not receiving help was also significantly larger (Wilkins 2006).
To sum up, growing shortfalls in the supply of formal and informal caregiving services in the future will put pressure on the provinces and territories to increase the amount of govern- ment-subsidized care they provide.
Second, there is great diversity in the care needs of seniors, and the range of services they require can be thought of as a continuum. At one end are people with mild disabilities and relatively easy-to-manage symptoms. At the other end are people with the most severe prob- lems and disabilities (MacKenzie, Hurst and Crompton 2009, 57). Accordingly, it is appropri- ate for governments to have different policies at different points in the care continuum.
People with lighter care needs will usually live in their own home or with family. Some may have a chronic condition that limits their mobility, in which case they may require homemaking and home support on a regular but infrequent basis. Others may be at home after spending time in a rehabilita- tion facility. They may need a range of homemaking and personal care services and perhaps further physiotherapy until their recovery is complete. Their need for care is thus likely temporary.
Those with intermediate care needs often have chronic conditions that have deteriorated to the point where their mobility is significantly limited. Others may be experiencing the first symptoms of cognitive impairment. (A study commissioned by the Alzheimer Society states that 55 percent of Canadians aged 65 and over with dementia live at home, and that the per- centage is expected to increase [2010, 7].) Individuals who are receiving post-acute care at home rather than in hospital may also be receiving intermediate care temporarily. Intermediate care services will, on average, be more numerous, more frequent and more spe- cialized than those required at the light end of the continuum. More often than not, people requiring this level of care are still living at home, although there are other options such as supportive housing and assisted housing. In either case, some of the assistance they receive may come from a provincial home care program, on either a subsidized or a nonsubsidized basis, depending on their income or that of a partner with whom they may be living.
The heavy end of the care continuum also encompasses a wide range of situations. The term “heavy” is used in this context to refer to the range and level of services required by individuals whose condition is both complex and of long duration, and thus very costly. This includes individuals who lack the physical or mental capacity to perform many of the activities of daily living without assistance; those whose cognitive impairment is severe enough to make communication difficult; those with severe behavioural difficulties; and those in end-of-life situations. Such individuals may reside in a tightly supervised group setting, a palliative care clinic, a long-term care facility or at home but with assistance readily available at all times. The term most often used by governments to describe the services required by people at this end of the continuum is “complex care” (see, for exam- ple, British Columbia 2010) or “complex continuing care” (see Ontario 2011). In a free- market setting, for people who require complex care for extended periods (years rather than weeks), the costs can be catastrophic, consuming all of their income and ultimately necessitating the sale of all their assets.
This diversity of needs is of course reflected in the types of care services required and the related costs. For some services the provider must have considerable education and train- ing. But many types of assistance require little specialized training and, as mentioned, tend to be provided by spouses, children, other relatives, friends, neighbours and volunteers on an unpaid basis. Some care recipients try to spare relatives and friends the time and effort of caregiving by purchasing services privately or obtaining them through public programs. Indeed, this may increasingly be the case as societal values and expectations begin to change (see Keefe, forthcoming).
Ultimately, there is a world of difference between the 65-year-old retiree with some modest limitations on her mobility married to a healthy man who takes on some of the physical chores that she previously performed, and the 90-year-old widow who has had advanced dementia for several years and is living in secure assisted housing with 24-hour surveillance. This suggests that government strategies should be flexible enough to respond according to the various needs at different points on the care continuum.
Third, individuals should plan their retirement with the expectation that they may need to pay for some care services, but planning for and financing catastrophic care costs is best done by pooling the risk at the societal level. Most people will require some form of care at some point in their later years, and in general there is no reason why they should not have planned their financial affairs during their working years such that they can pay for a moderate level of services in retirement. (This may not apply to the long-term unemployed or those with long- term dependence on social assistance or disability income supports.)
But that being said, it is impossible for most working-age individuals to know how much and what kinds of care they might need in their retirement years. This “unknowability” in terms of future care requirements raises important issues. It is unreasonable to expect indi- viduals to save enough during their working years to cover the relatively low probability but high costs of requiring prolonged, complex care.9 Yet we know that some individuals will face catastrophic care costs. The usual way for individuals to protect themselves against such a contingency is by pooling the risk through insurance. An important consid- eration is whether such insurance should be provided through the private market or social insurance.10
The Canadian Life and Health Insurance Association has estimated that 400,000 Canadians have long-term care coverage (CLHIA 2011). Given that there are about 18 million Canadians in the labour force and about 20 million between the ages of 20 and 64, it is clear that to date long-term care has been a relatively small market for insurers. Based on US studies, those who are most likely to need care in their postretirement years — those who develop chronic progressive illnesses or have permanent disabilities — are also least likely to be able to purchase insurance. High-income earners are also much more likely than low-income earners to purchase insurance for caregiving services.11
These and other particularities of long-term care and the market for private insurance sug- gest that social insurance is the best strategy (see Grignon, forthcoming). What is unknown in terms of risk and probability at the level of the individual can be estimated with much more certainty for the population as a whole. Available data make it feasible to estimate the longevity and morbidity of different cohorts. As new data become available, estimates can be revised and any resulting costs spread broadly rather than being absorbed by individuals. This social insurance role for public policy will be discussed more fully later in the study.
Fourth, notwithstanding provincial/territorial leadership in care policy, the federal govern- ment plays a useful, albeit almost exclusively indirect, role in this sphere. Various subsec- tions of section 92 of the Constitution Act, 1867 12 make it clear that each province is responsible for deciding what kind of care system it will develop, regulating that system, certifying the credentials of caregivers, fostering or developing the supply side (caregivers, institutions, etc.) and helping to ensure that it is funded. But the federal government is far from irrelevant. Federal powers related to taxation and old age pensions have considerable influence on the demand side of the care system. The federal spending power may also have affected the supply side through transfers to provincial governments, although the magnitude of any such effect is unknown. In short, on both the demand and the supply sides, the federal government has for the most part been an indirect player in the care system. Yet the anticipat- ed shortages of formal and informal caregivers will generate pressure on Ottawa to contribute financially to a solution.
Fifth, in deciding on whether and how it responds to these calls for financial support, the fed- eral government will have to take into account the economic status of seniors as well as the costs of care. But in fact, Ottawa lacks much of the information and analysis needed to make an informed and considered decision on the extent of its financial commitment.
Two kinds of information are required as a starting point. The first relates to the income and wealth of seniors in comparison with those of the working-age population. The government should not only have such information on a current basis, it should also have projections for the next two to three decades. The second concerns the costs of various care services, again looking ahead two to three decades.
The argument about the relevance of income and wealth is straightforward. Hypothetically, if the income of today’s seniors were double what it actually is, the vast majority of seniors would probably have the purchasing power to pay for much, if not all, of the care services they need.13 This stronger demand for paid care services would create incentives for both the voluntary and the business sectors to expand supply. In this scenario, the funding role of gov- ernments in care provision would assuredly be much smaller than is the case today.14 The opposite would apply if the current income of the elderly were half what it is.
In fact, Canadian seniors are now better off economically than they have ever been relative to the working-age population. The proportion of seniors with incomes below Statistics Canada’s low income cut-offs (LICOs) is less than half that of the population at large (Statistics Canada 2006a, charts 11-13). The proportion of seniors with low incomes after taxes fell from 10 per- cent in 1996 to 5 percent in 2006 (Statistics Canada 2008b). The main reason why so few sen- iors have low incomes is that the federal government’s Guaranteed Income Supplement provides benefits for couples aged 65 and older that are above the LICOs, although in some cases just barely above, depending on where the couple is living.
LaRochelle-CoÌ‚teÌ, Myles and Picot (2008) found that the median income replacement rate for all seniors in a cohort that they studied was equal to 80 percent of preretirement income. This exceeds the 65 to 75 percent replacement rate usually cited as the rate needed to maintain a standard of living in retirement equal to that experienced during one’s working years. They found considerable variation around the median, however, with over 20 percent of 75-year-olds having replacement rates below 60 percent, while 23 percent of those aged 69 to 71 had replace- ment rates over 100 percent. They also expressed concerns about whether current outcomes will be sustained in the coming decades — concerns that Wolfson (2011) has strongly reinforced. With respect to wealth, Statistics Canada reports that in 2005 the median net worth of families aged 35 to 44, 45 to 54 and 55 to 64 was $135,000, $231,000 and $407,000, respectively (Statistics Canada 2006b). The median net worth of those aged 65 and over was $303,000 and had improved relative to those of the other age cohorts since 1999.
This suggests that current seniors are faring reasonably well compared with the working-age population, although how adequate their retirement incomes will be when care expenses start to accumulate is another matter. Given the large proportion of elderly Canadians with disabili- ties reporting unmet care needs, it is probable that virtually all seniors with incomes below the LICOs, and many of those with incomes at or just above them, are unable to pay for private care services after retirement, even if they need only modest assistance. What is not known is how much of the reported care deficiency overall is due to shortages of caregivers, to seniors’ inability to pay for or access care services, or to other factors. To my knowledge, there has been no systematic assessment of the adequacy of the retirement income system in relation to the costs associated with different levels and durations of care.15 Future cohorts of seniors may fare reasonably well economically relative to the working-age population and yet have difficulty funding their care costs, given the policy status quo and the likely increases in the costs of care due to population aging.
The key point here is that the traditional analysis of the retirement income system has focused on two issues: its ability to prevent poverty and its effectiveness in enabling middle- income earners to maintain their living standards once they retire. A third question needs to be examined given ongoing demographic trends: the anticipated effectiveness of the retire- ment income system for future cohorts of retirees in relation to the anticipated care needs. Without such analysis there is little basis for Ottawa to decide what the extent of its contribu- tion should be, if any, remembering that there are many calls on the public purse.
Sixth and finally, as part of its strategy, Ottawa should concentrate on ensuring a better bal- ance between the demand and the supply sides of the care market. Demand-side measures are those that increase the purchasing power of the elderly and therefore their ability to buy the services they need in the marketplace. These include cash transfers and income tax provisions targeting seniors.16 Supply-side measures are government initiatives designed to add to the pool of care services, including formal and informal caregivers and various types of seniors’ accommodation. An example would be capital grants to increase formal caregiver training or the stock of appropriate housing. Indirect measures might include grants or subsidized loans, typically for the same purposes, but channelled through provincial/territorial governments.17
As will be seen below, the federal government concentrates almost all of its activities on the demand side. It may wish to continue doing so, premised on the view that a demand-side focus is the most appropriate way of respecting the constitutional division of powers. Whether it pursues or modifies its demand-side role, however, Ottawa should at least consid- er whether it has the means to leverage improvements on the supply side, in consultation with the provinces/territories, in anticipation of the caregiver shortages described above.
The classification of intergovernmental regimes is based on two sets of variables: the extent to which the federal-provincial relationship entails either independence or inter- dependence, and the extent to which it is hierarchical (coercive) or nonhierarchical (Lazar 2006). Figure 1 illustrates the classification system; each quadrant represents a distinctive form of federalism.
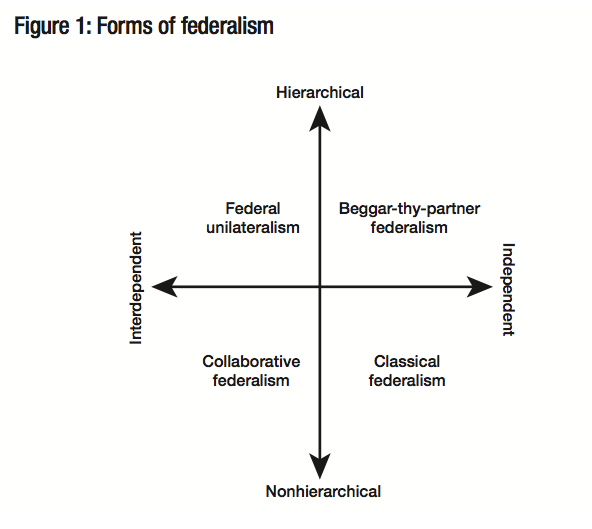
From the broad perspective of Canadian federalism politics, federal program initia- tives that fit within the two regime types below the horizontal axis tend to be rela- tively benign. Classical federalism occurs when one or even both orders of govern- ment are acting within their constitutional sphere, and the actions of one require little or no response from the other — this is sometimes called “disentangled” federalism. The federal role in defence and the provin- cial/territorial role in primary education are examples of governments acting within their areas of constitutional competence and requiring no response from the other order of gov- ernment. (This does not mean that these competencies are hermetically sealed from each other, as becomes clear when Ottawa closes a defence base or makes a major military purchase.) The advantages of this form of federalism are that it is consistent with the constitutional division of legislative powers, it makes accountability clear, and it avoids the heavy intergovernmental transaction costs that occur when there is extensive interaction between orders of government.
Despite these advantages, it should come as no surprise that in a world of growing functional interdependence, a lot of domestic program activity involves both orders of government. Collaborative federalism — when noncoercive federal-provincial/territorial relations are involved — can be very demanding. Examples over the last couple of decades include the Infrastructure Stimulus Fund, the National Child Benefit, and Canada Student Loans and Grants. Transaction costs are incurred in the form of heavy demands on the time of public ser- vants at both government levels and budgetary outlays for travel and communications. Collaborative federalism may entail negotiations that are never-ending, albeit with peaks and valleys, in much the way that the end of one round of collective bargaining in industrial rela- tions can lead almost immediately to the staking out of positions for the next round. Since collaborative federalism presumes no coercion, it is also analogous to efforts to manage inter- national relations without a hegemonic power.
While the effects of collaborative federalism on intergovernmental political relations are normally positive, and public opinion data frequently indicate that Canadians want their governments to cooperate, it is not uncommon to hear senior civil servants at both levels muttering privately that they would prefer the disentangled relationships that are more typ- ical of classical federalism.
Regimes above the horizontal axis are another story. They can create a lot of tension in the federation. Federal unilateralism arises when Ottawa exercises its spending power in an area of provincial/territorial constitutional competency without the uncoerced agreement of the provinces/territories. If Ottawa effectively coerces a province/territory to adopt a program that it otherwise would not have implemented through the incentives associated with matching grants, it is displaying federal unilateralism. The province/territory cannot afford to ignore the incentive, because if it does, its residents are effectively subsidizing Canadians in the rest of the country. Several provinces judged that Ottawa’s 2000 Affordable Housing Program, which was a matching grant program, entailed this kind of coercion. Of course, what some provinces/territories view as desirable federal uses of the spending power, others view as unde- sirable. The Quebec government has consistently rejected the idea that such a federal constitu- tional power exists (Quebec 1998), while the Alberta government has almost as consistently rejected its political legitimacy.
“Beggar-thy-partner federalism” is rare but not entirely absent from domestic intergovernmen- tal relations. It differs from federal unilateralism in that the initiative taken by Ottawa is within its constitutional competency. The coercion arises from the fact that the federal government’s action or inaction imposes costs on the provinces/territories with minimal discussion or con- sultation. For example, to the extent that the federal government does not provide or arrange for the provision of adequate services for “Indians, and lands reserved for the Indians,” for which it is constitutionally responsible (section 91 [24]), First Nations people who might have preferred to remain on reserve feel compelled to move off reserve to cities, leading to additional cost pressures on the provinces/territories for education, health and social services. It can also arise when Ottawa takes decisions to do more of something within its competency that effec- tively forces costs onto the provinces/territories. An example would be an amendment to the Criminal Code creating new offences, which adds administrative costs to provincial/territorial judicial systems without Ottawa negotiating to assume some share of those incremental costs.
The key objective of this study is to assess seniors’ care policy options for the federal govern- ment and their effects on Canadian federalism. But in the real world of government decision- making, many other assessment values or criteria are considered before a new social policy initiative is launched. Accordingly, potential policy options are examined from a broader pub- lic policy perspective, taking into account the following 10 criteria:
Notwithstanding the dominant role of the provinces/territories in legislating and regulat- ing care, Ottawa has had some influence on the way that caregiving arrangements have evolved in Canada since the Second World War. Although the federal role is significant, as noted above and as will be seen further below, it is almost entirely indirect. As the effects of population aging start to be felt in all regions of the country, the electorate will more than likely demand that the federal government do a lot more to manage the adjustments required. What in fact has Ottawa done historically, and what is it doing now?
Although there are particular groups for which the federal government has special respon- sibilities, including the growing number of war veterans and First Nations people on reserves, this section focuses on the broader issue of what the federal government’s role in caregiving has been for elderly Canadians, writ large, and how much additional policy freedom it has within the federal system. Table 1 lists the main policy instruments that Ottawa has used for purposes related to care or that have impacted on care, even if they were not intended specifically for that purpose.
Ottawa influences the caregiving system chiefly by shaping the country’s retirement income system and administering most of its largest programs. Even though provincial laws in respect of old age pensions constitutionally trump federal laws (see section 94A), Ottawa has historically been the lead political actor in creating the retirement income sys- tem. A principal source of income for current retirees is the public pension system. This includes Old Age Security (OAS), which dates from the early 1950s; the Canada Pension Plan (CPP) and the Guaranteed Income Supplement (GIS), both of which were enacted in the 1960s; as well as spousal and survivor allowances, which were developed mainly in the 1960s and 1970s. These are Canada’s largest statutory expenses and, including the Quebec Pension Plan (QPP), in 2008, they were paying out in the order of $60 billion annually (Finance Canada 2009, tables 10 and 39, adjusted to include CPP/QPP retirement pensions only). With regard to the CPP/QPP, it should be noted that these plans pay not only retire- ment pensions but also, and more significantly in terms of caregiving, disability pensions.
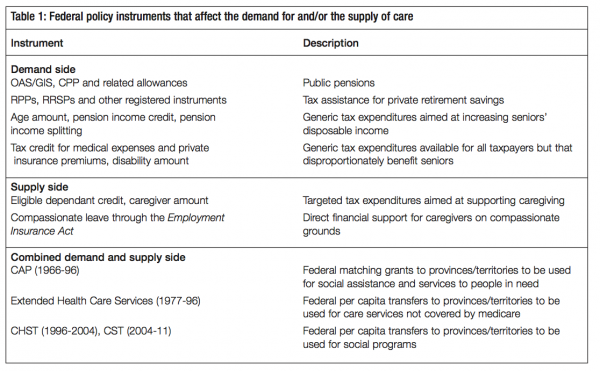
The federal government has also played a decisive role in encouraging private retirement sav- ings and pensions for current retirees, through income tax incentives for Registered Pension Plans (RPPs), Registered Retirement Savings Plans (RRSPs) and a number of related instru- ments. In the mid-2000s, these registered private plans provided over $40 billion annually in income to Canadian retirees and were growing more rapidly than the public plans. Gross fed- eral revenue forgone in 2009 for these two programs was close to $30 billion (Finance Canada 2009). The stock market sell-off in 2009 adversely affected this important source of retirement income, and the long-term effects of that event for future seniors remain uncertain.
Taken together, the public and tax-assisted private pension systems account for an estimated 60 percent of the income of people in their late 60s. This share rises to 70 percent for older seniors as the number of those still working dwindles.18 Compared with the situation in other OECD countries Canada’s public pension system has strong antipoverty characteristics, but it provides relatively weak earnings replacement for middle- and high-income individuals. While pension policy reforms are unlikely to focus on the highest earners, the middle-income groups are a potential target for improvements to the retirement income system.
Several provisions of the federal Income Tax Act also influence the income situation of seniors. The “age amount” can be viewed as a way of helping seniors fund their own care by recognizing that they must bear the added health-related costs of growing older, although, as with the OAS, the age amount targets low-income and low-middle-income taxpayers. The age amount was projected to reduce federal revenues by over $2.2 billion in 2009. The pension income credit (worth $945 million in 2009) and the relatively new pension income-splitting provisions ($730 million in 2009) have similar impacts in that they reduce the tax burden of retirees, leaving them better able to finance their needs (Finance Canada 2009).
There are other tax expenditures that are relevant to this discussion. For example, under the Income Tax Act, out-of-pocket medical expenses above a specified threshold for taxpayers or their spouses are eligible for nonrefundable tax credits. So too are the costs of private health insurance. Also, a “disability amount” can be claimed as a nonrefundable credit by persons certified as having a physical or mental disability that is severe and prolonged and requires care. The projected federal revenues forgone for medical expense tax credits and disability credits in 2009 were $945 million and $415 million, respectively (Finance Canada 2009). Obviously these two credits are not restricted to seniors, but they are more closely related to the demand for care services than, say, the age amount or the pension income credit.
Two small provisions have a clear supply-side focus. An “eligible dependant credit” is available to a taxpayer who supports and lives alone with a dependant in a home that the taxpayer maintains. Revenue forgone for that program in 2009 was projected at $765 million. There is also a targeted “caregiver amount,” which is a nonrefundable credit of up to just under $4,200 annually that a taxpayer can receive in respect of a close relative who is dependent on the tax- payer, if the dependant has a relatively low income. The projected cost of this provision to the federal treasury in 2009 was only $85 million.
In the context of this study, all but the last two of these tax provisions are generic in the sense that they are focused not on caregiving explicitly but on putting or leaving money in the hands of seniors or retirees, thus making it easier for them to purchase what they need, including care services. The fact that the current Conservative government has enriched these generic provisions by allowing for pension income-splitting and a doubling of the age amount suggests that its policy strategy has become increasingly focused on a demand-side approach. It is also a middle-class strategy, since essentially none of these credits is refundable (that is, they are of no value to low-income families and individuals who do not pay federal income tax), and they therefore do not help the poorest of the elderly.
While at first glance these tax expenditures, totalling about $5 billion annually, may seem sig- nificant, they pale in relation to the $60 billion annually in direct expenditures on public pensions and the more than $40 billion of private pension income derived from registered savings vehicles.
In summary, the federal government has a major impact on the demand side of the care sys- tem, even though its policies have not been established for that purpose. For all the big-ticket expenditures — and some of the smaller ones — in the retirement income system, federal poli- cy has not been designed with reference to probable care needs. Indeed, in a retirement income system that directly and through tax assistance provides roughly $100 billion of income annu- ally to Canadian seniors, perhaps 1 percent can be thought of as having some direct link to the demand side of caregiving. Yet, regardless of intent, Ottawa’s policies have a large influence on the size and distribution of the demand side of the care system for the elderly.
As for the supply side, historically the federal government has played at best a marginal role. (It may have had some indirect effect through the matching grant provisions of the Canada Assistance Plan [CAP], which will be discussed below, but with the disappearance of CAP in 1995, any such influence ended.) As with the demand side, the tax expenditures that current- ly target the supply side equal less than 1 percent of federal outlays for retirement income.
With regard to the effects of these federal programs on the federation and on intergovernmen- tal relations, one should bear in mind that while in the case of old age pensions Parliament has the explicit constitutional authority to legislate, provincial law prevails if there is a con- flict between the two orders of government. In this sense, Ottawa’s spending and tax expendi- ture programs for the current retired population are not coercive toward the provinces/territories. Indeed, apart from the intense intergovernmental negotiations in the 1960s that resulted in the CPP and the parallel QPP, the provinces/territories have generally looked to Ottawa to provide leadership in this area.19 This may be in part because the federal government has operational responsibility for public pension programs, but it is also because it has to concur with the provinces on CPP amendments.
The federal government has thus had a major indirect impact on the demand side of the care system for current retirees, and the situation can be expected to be the same for future retirees. The benign effect of federal retirement income programs on intergovernmental relations could remain unchanged as well. This is because the federal programs that underpin the incomes of all but the oldest of the current elderly are the same ones that will underpin the incomes of the future elderly. The CPP and the QPP are now mature programs and, in relative terms, their future growth will be linked mainly to population aging. The OAS and the GIS are not funded contributory schemes, and the statutory commitment to maintain the income they provide relative to wage growth is weaker than that for the CPP/QPP. But over the decades Ottawa has acted periodically to keep the real value of GIS benefits stable relative to wage growth (an easy task in recent years given the absence of real wage increases). In fact in the 2011 budget the government announced modest increases in the GIS. The key point here is that the federal government is acting within its constitutional powers in all of these pro- grams, which accounts for the benign intergovernmental relationship.
There are two reasons to think that this amicable relationship could change. The first is that over the past few years some of the weaknesses in the retirement income system have become more transparent. For people who were near their planned date of retirement when stock mar- kets tumbled in late 2008 (as a result of the international financial crisis), and who had been saving for retirement through RRSPs or defined contribution pension arrangements, their vul- nerability to the vagaries of the market became all too apparent. Deficiencies in supervision of defined benefit plans caused adverse effects on others when the pension plans of failed com- panies were terminated without sufficient assets to meet liabilities. At the same time, the low interest rates that have now prevailed for some time are having a drastic effect on the living standards of those seniors who draw a substantial portion of their retirement income from the interest on bonds and guaranteed income certificates.
These difficulties led some provinces to launch discussions with Ottawa with a view to enlarg- ing the CPP. In 2009 the Council of the Federation “called on the federal government to host a national summit on retirement income” (2009). In December 2010 six provinces requested that Ottawa “keep a modest CPP enhancement on the table as part of a package of reforms that would make saving for retirement easier, more affordable and more secure for Canadians” (British Columbia 2010). These provinces still appear to be interested in pursuing this idea, although the federal government and the other four provinces are seemingly less enthusiastic. In any case, if current concerns about declining RPP coverage and use of RRSPs and the diffi- culties with pension regulation are not addressed, the role of the CPP/QPP could be revisited (Ferley, Janzen and Onyett-Jeffries 2010; Baldwin 2011; Wolfson 2011). In such a scenario, intergovernmental tensions could arise due not to Ottawa intervening in provincial jurisdic- tion, but rather to provinces/territories pressuring the federal government to do more in an area of shared jurisdiction.
The second potential source of tension is the near certainty that rising care costs will put a strain on the budgets of the provinces/territories, causing them to pressure the federal govern- ment to help by transferring fiscal resources or otherwise absorbing part of the growing costs of care for seniors. This source of tension is of course linked to the first. If the deficiencies in the retirement income system prove to be more than transitory, the provinces/territories will be under even more pressure to increase their financial support of the care system.
The federal spending power is the main instrument Ottawa has used to provide assistance to the caregiving community. Historically, the most significant of its initiatives was the Canada Assistance Act, 1966. It authorized the federal government to enter into bilateral agreements with provinces to cost-share social assistance and social services on a 50-50 basis, provided that the assistance and services were for people “in need.” The initiative for CAP rested as much with the provinces as with Ottawa or more so (Osborne 1985). CAP was an improve- ment over the three categorical matching grant programs that preceded it. All provinces signed agreements with the federal government, which effectively left them free to define “need” as they saw fit, subject to commitments on interprovincial mobility, an appeal proce- dure and the requirement that the delivery agent of provincial programs be the province, a nonprofit agency approved by the province or a municipality. Ottawa’s basic role was to verify that expenses claimed by the provinces as eligible for cost-sharing were indeed eligible.
Seniors were not major beneficiaries of CAP. Relatively few persons aged 65 and over were considered in need, since federal GIS benefits generally assured them a higher level of income than that provided by provincial social assistance. As for CAP’s role in respect of services, this depended on provincial priorities. Given the age structure of the Canadian population in the 1960s and the fact that governments’ attention at the time was focused on establishing or developing medical insurance, post-secondary education and the retirement income system, care for seniors could not have been a priority for social service ministries.
Nonetheless, even though cost-sharing programs for seniors were but a small part of CAP, it was the main federal program for that purpose. Thus, Sherri Torjman points out that CAP cre- ated a “national legislative base for the support of social services,” including “essential support to help seniors and persons with disabilities to live independently in communities” (1997, 3). Yves Vaillancourt argues that CAP had a steering effect, in two ways: its cost-sharing provi- sions created incentives for Quebec and other provinces to focus their care policies on low- income families, possibly to the detriment of the middle class; and over time, CAP rules relating to delivery agents encouraged the growth of the third sector in Quebec, possibly at the expense of for-profit businesses (Vaillancourt 2003).
In terms of federal-provincial relations, it is safe to say that CAP, in and of itself, was relatively unobtrusive and less contentious than other matching grant programs of its era. But it was one of several federal matching grant programs introduced in the 1960s and, as we have seen, opinion was divided in the federation about the political legitimacy and, in the eyes of some, the constitutionality of using conditional grants to influence areas of provincial legislative competence under the Constitution (Tremblay 2000; Quebec 1998; Noël 2000a).
To address this concern, the federal government undertook not to introduce further programs of this ilk, and Parliament enacted the Established Programs (Interim Arrangements) Act, 1965 to remove some of the irritants of the conditional grant approach. This statute authorized Ottawa to enter into agreement with any province with which it had a cost-sharing arrange- ment, to enable that province to receive the federal share of costs in respect of certain estab- lished programs in the form of tax points instead of money. While opinions differ about the significance of this provision, at the time it enabled the federal and Quebec governments to deal with a political crisis in a manner that allowed both to claim satisfaction with the out- come (Kent 1988, 296; Vaillancourt 2003, 161). As is well known, only Quebec took up the tax-point offer at that time.
The 1977 fiscal arrangements saw the merger of federal transfers for hospital and medical insurance and post-secondary education into the new Established Programs Financing (EPF) block fund, with part of the federal contribution paid for in the form of a tax-point transfer. The 1995 federal budget merged CAP and EPF into the new Canada Health and Social Transfer (CHST) block fund. The CHST was subsequently, in 2003, decomposed into the Canada Health Transfer (CHT) and Canada Social Transfer (CST), both block transfers. In fiscal year 2011-12, the CHT and CST cash transfers will total $27 billion and $11.5 billion, and they are legislated to grow by 6 and 3 percent annually, respectively, until 2013-14.
Often neglected in the recounting of this history is the fact that the 1977 fiscal arrangements included a new program to cover extended health services such as nursing home intermediate care, low-level residential care for adults, health aspects of home care and ambulatory health services not covered in the federal-provincial hospital insurance agreements. The payment consisted of a per capita amount and an escalator. This was not all “new money,” in that the Extended Health Care Services program replaced some services previously provided for under CAP. This arrangement is noteworthy in that the federal government explicitly took on a funding role in relation to provincial care programs. Extended care was rolled into the CHST in 1996, and thus disappeared as a separate program.
So, what does this familiar history say about the current federal role in caregiving through intergovernmental transfers? With the end of matching conditional grant arrangements and extended care, there no longer is a federal instrument that serves as an incentive for the provinces/territories to build up their care systems.20 In fact, without the matching grant, there is no link between the CST and provincial care programs for seniors. Once received in provincial/territorial treasuries, the federal transfer dollars become fungible.
The federal spending power can also be used to transfer payments directly to organizations for the purpose of providing care to seniors. The evidence suggests that this option is not being seriously pursued. Human Resources and Skills Development Canada (HRSDC) currently administers New Horizons for Seniors, which acts as a clearing house for issues and ideas that pertain to caregiving, serves as an advocate for caregiving within the federal government, helps run the live-in caregiver program and transfers small amounts of money to community organizations that support a range of community-based initiatives to address social issues and barriers faced by people with disabilities (HRSDC 2009). The government announced in the 2011 budget that it was enhancing the New Horizons for Seniors Program with $10 million over two years to support projects that ensure seniors contribute to and benefit from activities in their communities (Finance Canada 2011).
In 2003 the Liberal government of Jean ChreÌtien amended the Employment Insurance Act to author- ize the payment of benefits to EI contributors for compassionate leave of up to six weeks to care for seriously ill relatives. To be considered seriously ill, a person must be “at risk of dying within 26 weeks,” as attested to by a physician. The benefits are aimed at caregivers involved in providing direct care, giving psychological support or arranging for care by a third party. Compassionate leave claimants in 2008-09 numbered just over 5,800. In total they received $9.9 million in bene- fits. This is a tiny program relative to retirement income programs and tax expenditures.
From a federalism viewpoint, this initiative is similar to the maternity benefits and parental leave provisions, whose constitutionality was challenged and which, notwithstanding their social poli- cy content, were ruled constitutional by the Supreme Court.21 There is little reason, therefore, to think the courts would view compassionate leave benefits differently. Thus it is appropriate, with- in the federalism classification system, to view this program as nonhierarchical, since it entails the federal government legislating in an area where it has constitutional authority.
All of the above federal policies, which entail legislation, regulation, spending or tax expendi- tures, can be viewed as hard policy instruments. The federal government also uses soft instruments, by commissioning reports, communicating information and research, and creating advisory bodies that may influence caregiving policies over the medium and long terms. The National Advisory Council on Aging is one example of a soft instrument. Established in 1980, it is mandated to assist and advise the minister of health (responsible for seniors) on all mat- ters related to the aging of the population and seniors’ quality of life. It issues periodic reports on matters of importance, but has little influence on federal policy. Its effects on the federal- provincial/territorial relationship are thus of no consequence.
The federal government also makes extensive use of task forces and commissions to structure debate on key issues. The reports of the Commission on the Future of Health Care in Canada (2002) (Romanow Report) and the Senate Standing Committee on Social Affairs, Science and Technology (2002) (Kirby Report) raised the profile of home care and caregiving. Regular reports from Statistics Canada on the country’s demographic trends more or less draw public attention to the emerging care needs of our aging society. Such soft instruments may be influ- ential in the long run, helping to inform and structure the debate, even if they seem to have little impact in the short run. In themselves, they have not been significant sources of tension in the federation.22
What kind of intergovernmental regimes do these various federal programs represent? How do the programs compare in terms of their potential effects on the federation? Figure 2 summa- rizes the analysis.
All of the federal programs are nonhierarchical, with the great majority falling in the classical federalism quadrant. Given the benign effects that programs below the horizontal axis have on intergovernmental relations, it is no surprise that current federal programs that have an impact on caregiving are not a serious source of intergovernmental tension — either because they allow governments to act independently of one another or because their interdepend- ence is well managed.
The programs that have involved the provinces with the federal government are the CPP/QPP and CAP. The CPP can, by law, be amended only with the agreement of the government of Canada and two-thirds of the provinces representing a minimum of two-thirds of the Canadian population. This puts the CPP into the lower left quadrant: collaborative federalism. Efforts made by all governments to maintain parallelism between the CPP and the QPP are also collaborative.
In the days of CAP, there was considerable federal-provincial interdependence, if only because the provinces designed and delivered programs while Ottawa paid half the freight and audited provincial spending. On policy matters, including social services such as caregiving, the feder- al government did not meddle. In any case CAP no longer exists, and its putative replace- ment, the CST, is at best a distant relative. The difference between the CST and CAP from a federalism viewpoint is shown in figure 2. CAP was a collaborative, province-friendly pro- gram. The CST is even friendlier, given that it allows the provinces and territories to use CST funds as they choose. The CST fits into the classical federalism quadrant.23
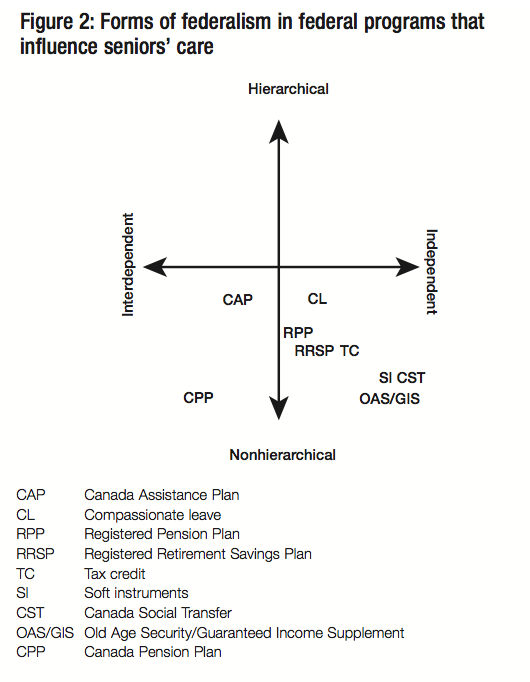
In the case of the OAS/GIS, the tax incentives for RPPs and RRSPs, and the various tax cred- its, Ottawa acts independently of the provinces/territories.24 These federal programs therefore fall into the classical federalism quadrant. The tax credits under the Income Tax Act are within federal constitutional com- petence, and Ottawa acts in this sphere whol- ly or largely independently of the provinces/territories when it uses this power. RPPs are also in the classical federalism quad- rant. They are placed very close to the vertical axis only because the treatment they receive under federal tax law is, in the majority of cases, linked to the plans being registered under provincial law for regulatory purposes. But in fact there is little interaction between the federal and provincial administrations, as each has a distinct regulatory role.
The compassionate leave program is also close to the vertical line, since it is likely that a fami- ly facing the circumstances that make it qualify for these benefits will also be interacting with provincial/territorial social services agencies.
Finally, the way in which the federal government uses soft instruments is within its constitu- tional authority. And it uses them largely independently of the provinces/territories.
The federal government has implemented programs that have potentially influenced the care- giving field in recent years, and in a fashion that does not interfere unduly with provincial constitutional competence. The words “have potentially influenced” caregiving have been carefully chosen. The dollar amounts associated with these programs are in the tens of bil- lions. In no way, however, do the larger programs focus explicitly on caregiving; they simply provide money to seniors that can be used for that purpose. As for the federal transfers to the provinces, even under CAP and extended health care, these never involved the federal govern- ment in deciding how much the provinces should or could spend on caregiving or the design features of provincial caregiving programs. And with the demise of these two programs, the federal government broke all links between the funds it transfers to the provinces notionally for social services, including caregiving, and how the provinces use those funds.
In a sense, the benign impact that federal policies have had on intergovernmental relations is not surprising. Ottawa effectively recognizes the constitutional role of provinces/territories in caregiving and has not, by and large, participated directly in this sphere of activity. In spite of this, it has had an influence through its large retirement income programs, which have helped to shape the demand side of caregiving. From a federalism perspective, the demand side of the caregiver market is much less susceptible to intergovernmental tensions than is the supply side.
For those who attach primacy to the Constitution and the importance of harmonious inter- governmental relations, this is what they would expect to see. They prefer that the federal authorities not meddle in provincial/territorial legislative jurisdiction. Implicit in this position is that they would expect the provinces and territories to continue stepping up to the plate and to introduce and implement care policies as necessary.
For those who focus more on public need than on the niceties of the Constitution and expect Ottawa to lead in the event of a Canada-wide social challenge, the federal caregiving policy cupboard must look bare. This is simply because the federal government has in fact no real policy that impacts directly and purposefully on caregiving, beyond its tiny compassionate leave program and its few tax credits (the eligible dependant credit; the caregiver tax credit; and tax support for home-based caregivers and for medical and disability-related expenses). The feder- al government announced an additional family caregiver tax credit in the 2011 budget — a 15 percent nonrefundable credit on an amount of $2,000 to provide tax relief for caregivers of infirm dependent relatives. The 2011 Conservative Party platform estimated the costs of this additional initiative at $160 million annually — which indicates that this credit will make lit- tle difference to the lives of most caregivers.
Before presenting the policy options available to the federal government, it is worth not- ing one of the reasons for making a distinction between options for light/intermediate care and those for prolonged, complex care. Since many seniors require light or intermediate care at some point in their later years, it is reasonable to expect people to have anticipated some of these costs and to have saved during their working years for this purpose. Put differ- ently, some of the options related to light and intermediate care place the onus on the indi- vidual, whereas, for reasons explained below, all of the options aimed at the heavy end of the care continuum depend mainly on the state. For those concerned about the overall private- public balance in retirement-related programs, this may warrant extra consideration of the pri- vate options for light and intermediate care.
Policy options for the light and intermediate points of the care continuum are presented first. They include both demand- and supply-side measures. Here, the range of options includes con- tinuing with established programs, variations on these and some new ideas. They all anticipate a growing need for care, but they do not specify dollar amounts except for illustrative purposes.
Clearly, some of the policies I have laid out below are not priorities today. But these options are not straw men. They are set out to help explore alternative strategic approaches, using both a federalism lens and a broader policy perspective that includes familiar policy criteria like equity and efficiency. The objective is to encourage the federal government to think strategically about the range of policy choices that are possible looking to the future. The options are presented in table 2 and discussed in turn below.
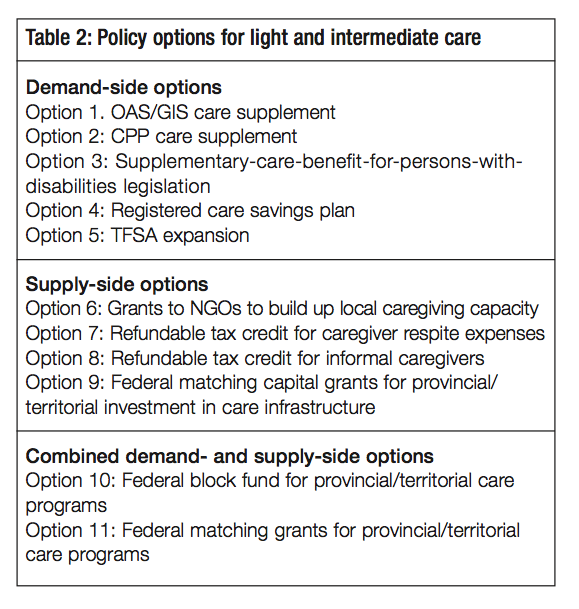
This option would enable OAS/GIS recipients to qualify for a supplement to their current benefits if their care costs exceed some mod- est deductible — say, $500 annually for some- one eligible for the maximum GIS and $1,000 to $2,000 annually if they receive OAS only. The supplement would cover 100 percent of care costs in excess of the deductible for those receiving the maximum GIS, and the percent- age of costs covered would gradually decline to zero as income increases. A ceiling of, say, $5,000 annually would apply. In designing this benefit it would be important to avoid an overall tax-back rate that would be punitive (although since this measure would not
mainly be focused on workforce participants, incentive effects would be less of a worry than is the case for stacked programs for people of working age). The tax-back rate might also be more gradual for seniors living alone than for those with a partner, to reflect the probability that they would have less access to informal care. Like the OAS/GIS, the care supplement would be funded out of general revenues on a pay-as-you-go basis. It could also be implemented quickly.
One risk associated with this option is that provincial/territorial governments could increase the co-payments they require from people who are in long-term care residences or receiving other subsidized services in order to capture the federal supplement. Accordingly, consultations with the provinces and territories would be necessary before such a measure could be implemented. From a provincial/territorial viewpoint, it would simply mean that GIS recipients, and perhaps those slightly beyond that threshold, would have additional income to purchase services. Even without adjusting their co-payment rates, the provinces/territories would have fewer seniors to subsidize under this option.
The rationale for such a measure is threefold. While relatively few elderly couples’ incomes are below the LICOs, a substantial number are only modestly above these levels, suggesting that they have little discretionary income, including for the purchase of care. Second, the problem is greater for unattached individuals who, because they lack a partner, do not have the finan- cial benefit of sharing accommodation or immediate informal care support should the need arise. Finally, seniors who rely heavily on the OAS/GIS are also the most likely to require provincial/territorial subsidies should they need care. With this care supplement measure, far fewer seniors would have to plead their case with provincial/territorial officials; they would be more autonomous.
This option could also be delivered through the mechanism of a refundable tax credit under the Income Tax Act.
Unlike the OAS and the GIS, which are linked antipoverty programs, the CPP and the QPP are intended to replace a portion of pre-retirement earnings. The benefits are very modest in size in that they replace only 25 percent of preretirement earnings, and only on earnings up to the national average wage ($47,200 in 2010). The design of these public pension plans was premised on the assumption that, during their working years, people would also avail them- selves of RPPs and RRSPs in order to have a retirement income sufficient to maintain their standard of living after retirement.
Like option 1, this option would put more money into the hands of seniors, contingent on their annual care expenses exceeding a deductible amount. But since the CPP is an earnings-related program, this care supplement would effectively target people with a stronger employment history than those targeted under the OAS/GIS option. As with the first option, the maximum supplement might be $5,000 annually (adjusted by a wage index). It would be funded through mandatory increases in CPP contribution rates.
Unlike option 1, the CPP care supplement would not be income-tested. It would be earned and paid for by the beneficiary as a contingent entitlement in much the way that CPP contributors are entitled to a disability pension under certain conditions. In other words, it would become payable when the beneficiary begins to incur care costs and could be modelled on disability benefits (combination of base amount and a contribution- linked supplement). Since it takes many years of contributions to pay for and thus earn a full benefit in a contributory plan, another important difference from option 1 is that full benefits would not become available for decades (how many is a design detail with vast financial implications).
Returning to the theme of intergenerational equity, if the full benefit were to come into force when the legislation is passed, today’s younger workers would have to pay higher contribution rates than are required to cover the costs of their benefits in order to compen- sate for older workers, who would have too few years to pay for their new benefits in full. The problem is that when today’s younger workers are ready to retire, they cannot expect to receive similar support from tomorrow’s younger workers. Given the current age struc- ture of the population, it would be unrealistic to assume what was assumed when the CPP and the QPP were introduced in the mid-1960s, which is that older workers could qualify for full benefits after a 10-year phase-in without putting an undue burden on younger workers or those not yet in the workforce. The idea was that the working-age population would subsidize the retirement pensions of older workers in the expectation that the chil- dren of that working generation would in turn subsidize their pensions. It was not expected at the time that the birth rate would fall as dramatically as it subsequently did and eventu- ally along with it the ratio of the population of working age to that of retirement age. It was also not realized how quickly the population would age. Based on current knowledge, a comparably rapid phase-in for a supplementary care benefit would be vulnerable to the charge that it is a Ponzi scheme.
Suppose the federal government wished to enact option 2 (CPP care supplement) but anticipated difficulty securing the necessary provincial approval for a CPP amendment. It could pursue the same policy outcome by using a different instrument. The same substantive supplementary care benefit as in option 2 could be enacted in separate legislation, referred to here as the “supplemen- tary-care-benefit-for-persons-with-disabilities act.” The choice of name would make it clear that it was being enacted under section 94A of the Constitution, which reads: “The Parliament of Canada may make laws in relation to old age pensions and supplementary benefits, including survivors’ and disability benefits irrespective of age, but no such law shall affect the operation of any law present or future of a provincial legislature in relation to any such matter.”
As in option 2, this option calls for prefunding. Contributors would not earn a full benefit until some relatively distant future date, depending on the design. In this case, a new payroll tax would be levied and the money raised would be placed in a fund separate from the CPP Fund and the Consolidated Revenue Fund. Any province opposed to the legislation could take advantage of the provincial paramountcy provisions noted above and not participate. In that event the tax would not apply in the nonparticipating jurisdiction. Two mechanisms for non- participation are possible: opting in and opting out. Opting in means that the federal legisla- tion would come into force in a province or territory only when that jurisdiction notifies Ottawa that its legislature has voted to participate. Opting out means that the federal legisla- tion would apply in all jurisdictions unless the legislature of a province or a territory votes against participation. The opt-in procedure is more province-friendly. The opt-out procedure is more robust from a caregiving policy perspective.
At the federal level, an important question would be whether Ottawa would proclaim such legislation into force if only two or three provinces signal their wish to participate. In all prob- ability it would not. But by proceeding in this way, it would be demonstrating that it is willing to accept a lesser measure of provincial consensus than the CPP amendment rule, which requires agreement from at least seven provinces representing a minimum of two-thirds of the Canadian population. The Social Union Framework Agreement (SUFA) rule for shared-cost programs requires only agreement from a majority of the provinces without stipulating a min- imum share of the population, but this is not a shared-cost program. To amend most constitu- tional provisions a 7/50 rule prevails (that is, at least seven provinces representing at least 50 percent of the Canadian population must formally approve).
There is rich precedent for these opt-in/opt-out measures in the history of medicare. When Louis St-Laurent became prime minister in 1948, he inherited a Liberal promise of a compre- hensive, publicly insured health care system, and there was a commonly held view that the first step in public insurance should focus on hospital insurance and diagnostic services. But he personally was not a supporter. In his second mandate, St-Laurent was cajoled by some of his ministers and some provinces to modify his position, but he dragged his feet. At a 1955 federal-provincial conference, St-Laurent stated that he did not consider it appropriate for Ottawa to impose taxes on all Canadians when only one, two or three provinces representing a distinct minority of Canadians were eager to proceed with hospital insurance. He went on:
“But if there were a substantial majority of provincial governments representing a substantial majority of the Canadian people who were prepared to embark upon provincially adminis- tered health insurance schemes,” then the federal government would play its role (Taylor 2009, 212). At the time, in 1955, such a “substantial” majority had not yet emerged. Hospital insurance legislation was introduced by the St-Laurent government shortly before the 1957 general election with a 6/50 rule. Although the Bill was enacted, it was not brought into force before the Liberals were defeated in the general election of 1957. When John Diefenbaker’s Progressive Conservatives won office they introduced an amendment to drop the threshold from six provinces to five, and the legislation came into force.
When it came to medical insurance, the government of Lester B. Pearson took the opposite tack. It declared that once legislation had been passed, federal cost-sharing would begin, even if there was only one province ready to take advantage of Ottawa’s matching grants.
In short, there is ample precedent for any of a number of rules. From an intergovernmental relations perspective, option 3 would acknowledge that the federal authorities lack the con- sensus to secure a CPP amendment but wish to move forward without that measure of sup- port. In itself, that lack of provincial support would be controversial. This could be a minor and short-lived controversy, or it could flare up into a major flashpoint. The best way to mini- mize the risk and still proceed would be to adopt the opt-in process with something like a 6/50 or 5/50 rule. The legislation might not be promulgated for several years, but this is an issue for the long haul.
While RRSPs are disproportionally used by higher earners, this proposal would encourage modest- to middle-income earners to save for their future care needs. The registered care savings plan (RCSP) would be similar to an RRSP (providing tax deduction and shelter with taxes paid on with- drawals) and its deduction ceiling would be integrated with RRSPs and RPPs to limit maximum tax deductions. But it would differ from the RRSP in several important ways. First, the federal gov- ernment would contribute directly to RCSP accounts, on an income-tested basis, up to $5,000 to $10,000 over the lifetime. These grants would be similar to those currently provided in conjunc- tion with the Registered Disability Savings Plan (RDSP).25 Second, withdrawals would be allowed only to cover eligible care costs. Third, the logical consequence is that RCSP accounts could remain intact until death, at which point the accumulated funds would be taxable as part of the estate of the deceased. This would not only enable the healthy plan participant to enjoy the bene- fits of sheltering the earnings of her account until a very old age, but also require her to do so.
For a contributor, the advantages would be the federal cash contributions and the longer tax shelter period relative to RRSPs. These advantages are intended to outweigh the disadvantage of less withdrawal flexibility. For the federal government, the objective would be to encourage people to better prepare for the financial costs of care. The hope would be that, by the time a person has “maxed out” on the federal cash contribution, saving for future care needs has become a habit. This approach would likely reduce the need for provincial/territorial subsidies for caregiving services, since seniors would be able to afford a larger share of the costs.26
The Tax-Free Savings Account (TFSA), established in 2009, is a new way for Canadians to set money aside tax-free throughout their lifetime. Contributions to a TFSA are not deductible for income tax purposes, but the initial amount contributed as well as the income earned in the account (for example, investment income and capital gains) is tax- free, even when the cash is withdrawn. The contribution limit is $5,000 annually, indexed to the inflation rate. Option 5 consists of raising the TFSA limit significantly (to, say, $7,500 or $10,000) to help people save for the day when they will need extra money for care services or some other necessity.
This approach has three advantages. First, as noted above, there is a need to maintain a public-private balance in the retirement income system, and TFSAs could expand the pri- vate side. Second, TFSAs are a more advantageous way for modest- and middle-income earners to save for retirement than RRSPs and RPPs, mainly because the income they pro- vide after retirement is not taxable and therefore not taken into account in determining eligibility for and the tax-back of OAS/GIS benefits (see Horner 2011).27 Third, the TFSA is much more flexible than the RCSP. Its disadvantage flows from this flexibility: There is no guarantee that it will be used to purchase care services. The 2011 Conservative Party elec- tion platform announced the government’s intention to raise the TFSA limit to $10,000 annually once the federal budget is balanced.
To sum up, four of the demand-side options for light and intermediate care are within federal legislative authority. The fifth, the CPP care supplement (option 2), would necessitate an amendment to the Canada Pension Plan Act, which, as noted, would require the support of seven provinces and at least two-thirds of the population. If the CPP and QPP are to remain parallel, it would also be necessary to amend the QPP Act. The federal government could implement and administer all five options with little difficulty.
The purpose of the grants would be to increase the number of caregivers. The federal spending power would be used to provide operating funds to nongovernmental organizations (NGOs) conditional on the NGOs using them to improve the supply of care services for seniors on either a nonprofit or a for-profit basis and according to various provincial/territorial certifica- tion and regulatory standards.
The NGO would not itself become a caregiving entity but rather would encourage new firms to enter the caregiving business by supplying information on local demand and supply of care workers, provincial/territorial occupational standards and training programs for care- related occupations. Where these don’t exist, it would work with labour market partners to set standards and develop training programs. The NGO could also eventually act as an employment agency matching potential employees with caregiving jobs. With this kind of basic information provided at little or no cost, a significant start-up cost for small entrepre- neurs would be subsidized.
For this option to have impact, the program would have to be larger than other grant and contribution programs run by the relevant federal department, HRSDC (HRSDC 2010a, 2010b). Yet if the program is very large, it would compete directly with the provinces/territo- ries within their jurisdiction. Conversely, if it is small, it would risk irritating the provinces/territories while having little effect. An intermediate option would be to target a region in the province or territory where care services are in shortest supply. The grants might run for, say, three to five years while regional capacity is being developed. The selection of tar- get regions would proceed in full consultation with the province.
To be effective, this option would also require a commitment from the provinces and territo- ries that they will not reduce their caregiving expenditures as Ottawa ramps up its contribu- tion (i.e., “no displacement”).
Informal caregivers play a huge role in today’s care system for seniors, and as the popula- tion ages, the need for care providers will increase. Reports on informal caregivers consis- tently point to the lack of support and relief as an important source of stress and fatigue (see Keefe, forthcoming). The Canadian Institute for Health Information reports that about one-third of caregivers assisting a person with moderate to severe cognitive impairment feel distressed (CIHI 2010, 10).
The objective of this measure would be to make it easier for care recipients to hire a substitute caregiver while their regular informal caregiver is on leave. Under specified conditions, the care recipient would be eligible for a refundable tax credit for costs incurred. This would facilitate the caregiver taking time off for respite without fear of leaving the senior in the lurch. Note that this option is more appropriate for individuals requiring intermediate or complex care, as by defini- tion persons with lighter care needs would not require as many hours of personalized care.
Eligibility requirements for this credit might include a condition that the unpaid caregiver has been providing care services regularly for a minimum period, perhaps as short as three months. The value of the credit could be calculated so as to enable the senior to purchase an amount of respite care equal to a percentage of the regular caregiver’s work time.28 For example, if the caregiver normally provides 100 hours of care monthly, then the credit would not exceed an amount equal to a fixed percentage of those 100 hours, perhaps somewhere in the range of 15 to 20 percent, multiplied by the hourly rate required to hire the respite caregiver. The source of funding for this credit would have to be worked out among the federal, provincial and territorial governments, but in principle the funds should come from Ottawa.29
The objective in this case would be to increase the number of informal caregivers substantially relative to the status quo. Based on current knowledge it is difficult to know how big an incen- tive would be required to make a difference and what the overall cost would be. Therefore it might be wise to test different models with pilot projects.
There are many design features that would have to be tested, but the idea would be to find the optimal level of incentive required to have a significant impact on supply, without doing preju- dice to other parts of the economy. Since the paid labour force will be shrinking in relative terms as society ages, the incentive should not be so large as to create undesired labour market effects. The program might target individuals who have recently retired, those who have relevant experi- ence but are not currently employed, and family members of care recipients. Eligibility would be restricted to those providing intermediate to complex care. The credit would also be income- tested. This is consistent with Kershaw’s proposal to “enrich the existing caregiver tax credit and redefine it as a refundable caregiver credit” (Kershaw 2002, 1950).
This option overlaps with the existing caregiver credit and the eligible dependant credit. These two provisions offer tax relief to relatives providing in-home care. The existing tax provisions have been described as “but a ‘symbolic gesture’ in terms of valuing unpaid caregiving labour” (Canadian Centre for Elder Law 2010). The proposed credit differs from those provisions in two ways. It would be refundable. And there would be no requirement that the care recipient and the caregiver live in the same residence or be related to one another. Compared with the current caregiver measures, this option would be more expensive in terms of revenue forgone, but it would still be a relatively inexpensive way to reduce unmet care needs and it could reduce the need for more costly formal care. Finding more effective ways to support informal caregiving will become even more important in coming years, given the growing caregiver shortages that are anticipated.
Provincial governments have had their toes in these waters for some time, but without any sense of urgency. In 2009 the government of Nova Scotia announced the creation of what was reported to be the only existing direct allowance for family caregivers in Canada (Nova Scotia 2009). The Allowance to Aid Caregivers is an income-tested $400 monthly benefit for eligible caregivers who perform 20 hours or more of care per week. The care recipient must be assessed as having a signifi- cant impairment. In 2010 the government of Manitoba announced the Primary Caregiver Tax Credit, an annual refundable tax credit that can be claimed by a person who is acting as primary caregiver without pay for a family member, friend or neighbour requiring level-2 care or higher under the Manitoba Homecare Program guidelines. The caregiver can claim $1,275 a year per care recipient, for up to three care recipients (Manitoba 2010). Several other countries offer much greater financial support for caregivers than Canada (Canadian Centre for Elder Law 2010, chap. 6).
Since the shortage of caregivers and care facilities is expected to grow, the federal government could introduce a time-limited program of capital grants to the provinces and territories for the purpose of building up the supply side, both physical plant (e.g., more assisted living accommodation) and human capital (e.g., training programs for care workers).30 The provinces and territories are responsible for managing the care system, and the most efficient way for Ottawa to promote growth of the supply side is to work with and through them. This approach would leverage federal money. The National Health Grants Program (1948-71) could be a model; it was also a 50-50 matching grant program. To ensure that option 9 serves its intended purpose, the grants would be applicable only to provincial/territorial spending that is incremental to current or currently planned levels. This program would be developed col- laboratively by the two orders of government in a manner consistent with the provisions of SUFA, which will be discussed further below.
The next two options entail establishing a new federal conditional cash transfer to the provinces and territories to help them finance programs and services to address the grow- ing care needs of seniors. The rationale for this approach is that the federal government can best advance its agenda for care by providing a specific-purpose grant to the jurisdic- tion that has responsibility for care programs. The federal government would seek to devel- op the seniors’ care transfer in collaboration with the provinces/territories in a manner consistent with the provisions of SUFA. To the extent that the provinces/territories use the federal funds to subsidize more clients, this would support the demand side of care. To the extent that the funds are used to hire more caregivers or provide training for existing care- givers, the supply side would benefit.
Both options would require the following initial steps: (1) In consultation with each jurisdic- tion, establish the provincial/territorial per capita operating costs for seniors’ care in a given base year; (2) determine the size of the federal transfer for year 1; and (3) decide on the growth formula to be applied to the transfer amount of year 1 in order to calculate the transfer amounts for years 2 and beyond. The escalation method is what distinguishes the two options.
The main question is, what determines the size of the federal transfer in year 1. In reality, there is no magic formula for establishing a “fair” amount based on some objective set of criteria. The year-1 transfer would have to be an amount that Ottawa judges sufficiently large to be accepted by the provinces/territories with its accompanying federal conditions. The main condition might simply be that the provinces/territories agree not to reduce their spending for seniors’ care below the sum of their base-year per capita operating outlays plus the per capita funds received from Ottawa. The purpose would be to ensure that the new federal transfer is used solely for its designated purpose — to enhance care for seniors — otherwise the effect would simply be to shift federal revenues to the provinces/territories’ consolidated revenue fund for other priorities. From Ottawa’s perspective, the object would be to leverage its money for a growing social need. From the provinces/territories’ perspec- tive, a key issue would be whether the conditions attached to the transfer are so onerous as to outweigh the value of what could be seen as a windfall.
The initial block transfer amount would be determined through negotiation, and in subse- quent years escalated by a pre-established rate of increase not explicitly tied to provincial/territorial outlays. The escalator could be the rate of GDP growth or any indica- tor other than the actual increase in provincial/territorial spending to ensure that federal transfer increases are not driven by that spending. This would also avoid the need for Ottawa to audit provincial/territorial expenditures subject to some broad intergovernmental understanding about how to ensure that there is no displacement.
This operating grant would leave it to the provinces/territories to decide how to use the incre- mental federal funds within the seniors’ care envelope, subject to a few conditions. Apart from a “no displacement” provision, the conditions could include mobility/portability provisions and an agreement to meet some minimum care standards negotiated by the two orders of government.
The only difference between options 10 and 11 is the escalator. In this case, the escalator would be a matching grant on all per capita expenses incurred by the jurisdiction above its per capita seniors’ care expenditures in the base year. Thus, if a province/territory spends $100 per capita in the base year and $103 in year 1, the federal government would cover, say, half of the $3 per capita increase.
Ottawa might prefer this escalator, because it would be an incentive for the provinces/territo- ries to give higher priority to seniors’ care programs (costing the jurisdiction only 50 cents for each dollar spent). Moreover, one traditional federal government objection to matching grants — that Ottawa loses control of its own spending — would have little relevance in this case. This would be a concern if Ottawa were providing matching grants on a large initial base, such as a province/territory’s total social services or education budget. But addressing the care needs of seniors takes up only a small fraction of the budget of the social services or health ministry responsible for these services. Escalating this sum annually on a cost-matching basis would not jeopardize federal control of its overall budget. Also, since this would be a match- ing grant, it is assumed that Ottawa would put a cap on federal outlays.
If the federal government entered into such agreements with the provinces/territories, there would probably be a legal obligation to audit the jurisdictions’ expenditures, to ensure that they are in fact eligible for cost-sharing. The provinces/territories, however, would likely prefer the block funding option because the 50-cent dollars would be seen as distorting their priori- ties, and because the audit provisions would be viewed as too intrusive.
In this section, the policy options for light and intermediate care are assessed, first in terms of their probable effects on Canadian federalism — which is the dominant concern of this study — and second within a broader policy assessment framework.
This analysis leads to a few simple questions: Are there options that would not be irritants to the federation and to intergovernmental relations and that would also do well on the 10 poli- cy criteria? If so, are there options on both the demand and the supply sides? Are there options that would appeal to a market-oriented, conservative government, a centrist govern- ment and a social democratic government?
Figure 3 provides a snapshot comparative assessment of these 11 options as seen through a federalism lens. While the upper left quadrant is labelled “federal unilateralism” in figure 1, some might describe it as the “strong federal government” quadrant, in that the programs that fit into it are based on the idea of Canada as a sharing community. Option 11 (federal matching grants for provincial/territorial care programs) is identified as potentially the most coercive, because it would effec- tively require the provinces/territories to accept federal priorities in an area of provincial jurisdiction. In the case of the block fund transfer, option 10, the extent of coercion would depend on the condi- tions that are attached. Whether these two transfer options are in fact coercive would depend on the process followed by Ottawa in seeking provincial/territorial support and the way in which each jurisdiction defines its own self-interest. If the federal government undertakes minimal consultation and then announces its proposal, knowing that only a few provinces/territories are interested, the effect on overall federal-provincial/territorial relations could be poisonous.
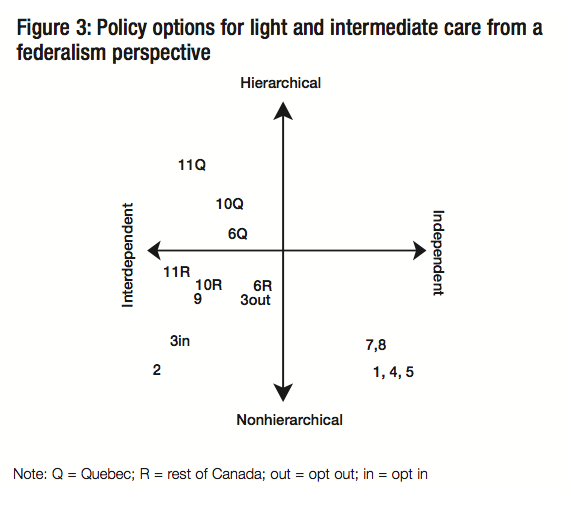
By contrast, if a process similar to that set out in section 5 of SUFA is followed — that is, both orders of government collaborate in identifying priorities, the federal government obtains the agreement of a majority of provinces before introducing the proposed shared-cost or block-fund- ed program, and the two orders of government agree on an accountability framework — then the impact on intergovernmental relations would be less adverse and possibly even cause for cel- ebration (Social Union Framework Agreement 1999). Nonetheless, there will almost always be at least one jurisdiction that does not want to participate in such an initiative yet is compelled to do so, because it would find it hard to explain to its population why they are paying taxes to Ottawa while a share of that money is not flowing back to their province or territory.
In the event that Ottawa undertakes a SUFA-consistent process, some provinces/territories would probably view options 10 and 11 as collaborative and welcome them. In contrast, based on previous reactions of Quebec governments to federal initiatives involving the spending power, it is virtually certain that Quebec would take strong objection to both options 10 and 11 — the only question is how strong (Noël 2000b). This is why in figure 3 these two options are shown for Quebec (“Q”) and for the rest of Canada (“R”). Depending on circumstances, one or two other jurisdictions might also resist Ottawa’s overture, due to different opinions about the nature of the federation, differences in provincial/territorial priorities and/or eco- nomic and fiscal conditions, or even political considerations.
Under SUFA, jurisdictions that are not part of the majority that has agreed to a new Canada- wide federal initiative but that “meet or commit to meet the agreed Canada-wide objectives and agree to respect the accountability framework will receive their share of available fund- ing” (SUFA 1999, section 5). To understate the facts, for the nonagreeing provinces/territories this condition is not a high hurdle. At least in respect of larger federal transfers, it has been decades since any jurisdiction did not receive its “appropriate” share of federal funding in a joint program.31 Thus, if Ottawa does proceed with either of these two options it is highly probable that Quebec would opt out and still receive its share of the funding.
SUFA is a political agreement between the government of Canada and the governments of all provinces and territories (at the time) except Quebec. It is not legally binding. After the agree- ment was reached, it dropped out of sight (Fortin, Noel, and St-Hilaire 2003). Political leaders virtually never refer to it publicly, perhaps because it was never accepted by Quebec. Nonetheless, its principles and the procedures it calls for are a good way to conduct intergov- ernmental relations. Since the 2004 federal-provincial/territorial Health Accord, under the Martin government and especially under the Harper government, there appear to have been few egregious transgressions of SUFA’s broad principles.32
At the same time, although the form and substance of intergovernmental relations embodied in options 10 and 11 have been common in post-Second World War Canada, they remain objectionable to the government of Quebec. Quebec holds the view that federal- provincial/territorial agreements that rest on the spending power are not consistent with the division of legislative powers as set out in the Constitution. Over the decades, Quebec govern- ments of all political stripes — Liberal, Parti QueÌbeÌcois and Union Nationale — have argued that the spending power is a fiction and that it has no basis in the Constitution (Quebec 1998). As a result Quebec often opts out of joint programs or participates in an asymmetric fashion. In some cases it may hold its nose and participate. Whichever of these positions Quebec takes, the government of Canada ends up paying the government of Quebec its share of the federal transfer and there is usually considerable ambiguity in the public communica- tions that follow, with Ottawa and Quebec each putting its spin on the outcome. In consider- ing its strategy in respect of care policy for seniors, a big question for Ottawa is whether damage would be done to Canada-Quebec relations if option 10 or option 11 is pursued and, if so, how much damage. It could be a little, or it could be a lot.
Quebec is not the only jurisdiction to challenge the federal role in using the spending power. The government of Alberta has consistently questioned the legitimacy of this role since the time of the Lougheed premiership (Alberta 1978a, 14-15; Alberta 1978b, 78-81). Periodically, particu- larly when the Conservatives are in power (or, previously, the Progressive Conservatives), Ontario has taken the same position. The other jurisdictions are more interested in seeking con- trols on how the federal spending power is used, and in imposing some limits on Ottawa’s dis- cretion on “dis-spending,” perhaps through a constitutionalized, modified version of SUFA. Such a provision was included in the failed Meech Lake and Charlottetown accords.
The key message here is that the federal government could try to proceed with the cost-shar- ing arrangements in options 10 and 11 and adopt more or less openness and flexibility in the negotiating process. But it will always be important for Ottawa to be satisfied that it cannot reach its objectives in other ways. Would the benefits of implementing a new block fund (option 10) or matching grant (option 11) for seniors’ care be worth the risk, in terms of the impact on intergovernmental relations and the state of the federation?
Returning to figure 3, option 9 (federal matching capital grants for provincial/territorial investment in care infrastructure) is shown well below the horizontal axis even though it, too, is a matching grant program. The provinces/territories are generally more open to matching- grant agreements that involve capital expenditures than they are to those that pertain to ongoing provincial/territorial operations. For one thing, matching grant agreements are invariably time-limited, which means that the federal presence will also be time-limited. As well, joint programs that are for capital investment purposes carry much less risk of Ottawa intruding in the daily program administration of provinces/territories than do conditional grants for operating purposes.
The options in the lower right (classical federalism) quadrant would enable the federal govern- ment to act independently of the provinces/territories. For example, option 1 (OAS/GIS care supplement) would entail incremental federal spending in an area in which Ottawa has the constitutional right to legislate, and it would not put pressure on the provinces/territories to change their priorities. Options 4 and 5 are income tax measures within federal jurisdiction. All three are demand-side measures. Options 7 and 8 are also tax measures, but they are aimed at influencing the supply of informal caregivers. While neither would be an intrusion into provincial/territorial affairs, both are located a little closer to the vertical and horizontal axes by virtue of the fact that they would intersect more directly with provincial programs than the demand-side measures.
Option 2 (CPP care supplement), which appears in the bottom left (collaborative federalism) quadrant, is highly interdependent and noncoercive because of two factors: the strict federal- provincial consensus formally required to amend the CPP Act, and the Quebec/rest of Canada political consensus to minimize differences between the QPP and the CPP.
Perhaps the most difficult option to assess for its effects on the federation is option 3 (sup- plementary-care-benefit-for-persons-with-disabilities legislation). From the viewpoint of policy substance, both the opt-out and the opt-in variants would allow a province/territory to not participate, in which case its residents would not be taxed to fund this benefit. Nonetheless, the optics would be different depending on which variant is chosen. If the law automatically applies to all provinces unless they opt out by having their legislatures vote on the issue, any province that is opposed would have to publicly stand up and declare its nonparticipation. If the opposition parties in the province do not share the gov- ernment’s view, the issue could readily become a problem for the government in question. If the legislation is drafted on an opt-in basis, it would be politically easier for the province that wishes not to participate. The opt-out and opt-in variants are shown separately in fig- ure 3.
Option 6 (grants to NGOs to build up local caregiving capacity) would be less controversial and sensitive than intergovernmental transfer agreements, in part because it would not require matching grants from the province/territory. For Canada outside Quebec, the effect on intergovernmental relations would likely be small — it would likely prompt a mix of welcome, indifference and possibly mild irritation. On the whole, most provinces would welcome such an initiative if there are meaningful consultations on the program design at the outset and on the selection of targeted regions once the program is up and running.
Based on historical precedents Quebec would likely object. The most famous precedent is the Duplessis government’s opposition to a program of federal grants to Canadian colleges and universities during the 1950s. The province won the dispute in the political arena, and Ottawa agreed to transfer corporate tax room to Quebec in lieu of the direct transfers. Since then, Quebec has consistently opposed federal transfers to post-secondary institutions, including those for purposes such as adult education, training, continuing education and support for students (Quebec 1998). For the government of Quebec, the normal response to such an ini- tiative would be that caregiving is under Quebec jurisdiction. If the federal government has enough money to be spending in provincial jurisdictions, this merely demonstrates that it has occupied too much tax room. The federal government should lower its tax take, so that Quebec (and any other province or territory that so desires) can increase its revenues while leaving the Quebec taxpayer neutral.
The grant program proposed here is on a significantly smaller scale, however, than the 1950s precedent was, and it would probably have a modest public profile. Thus, although Quebec would likely object, its objection might be tempered, or even pro forma, if it is able to exercise substantial influence over the region selected.
Since option 6 would require intergovernmental collaboration, it is located on the left side of fig- ure 3. Quebec would view it as intrusive and an irritant but not coercive unless it is implemented on a large scale. Hence it is located above the horizontal axis, but only just. For the ROC it is located below the horizontal axis. Option 6 is on the margin, from a federalism perspective.
The 11 policy options for light and intermediate care have also been assessed against 10 policy criteria using a simple rating system that gives all criteria equal weight.33 This assessment is presented in tabular form in appendix 1. The bottom row summarizes the ratings. The five demand-side options and three of the supply-side options (7, 8 and 9) were assessed as the best. These eight policy options were all assessed as “good” or higher on seven of the ten assessment criteria. In contrast, options 10 and 11 were rated as “fair” or “poor” on four crite- ria. Option 6 was rated “fair” or “poor” on seven criteria. Importantly, the three options that received lower ratings on the policy criteria all raised significant questions in my earlier dis- cussion of their effects on federalism.
At this point it may be useful to recall that the purpose of this study is to form a view on how much freedom the federal government has in fashioning a policy strategy for seniors’ care, not to propose an optimal care policy strategy. As was noted, from a federalism perspective options 10 and 11 are problematic and option 6 is at least suspect. If these three options had scored best on the 10 policy criteria, and if the eight options that are robust from a federalism viewpoint had scored very poorly on the policy criteria, the federal government would be heavily constrained.
But the opposite is the case. There are demand-side and supply-side options that do not raise red flags from a federalism viewpoint and that received positive policy assessments. The kind of federalism implicit in demand-side options 1, 2, 4 and 5 is benign. The opt-in version of option 3 is also respectful of provincial paramountcy and ought not to raise provincial hack- les. Options 1 to 5 also scored well on the policy criteria. A federal strategy that includes one or more of them could thus be described as win-win (good federalism/good policy). Options 7, 8 and 9 are supply-side options that are also benign from a federalism perspective and were assessed positively on the policy criteria.
At this broad level of generality, two points emerge. For the light and intermediate points on the care continuum, there is scope for a federal policy strategy that is oriented to either the demand side or the supply side, or both. However, the range of choices is richer on the demand side, in part because the supply-side programs come closer to touching provincial jurisdiction. These conclusions are summarized in table 3.
The analysis can be taken a step further. Most of the policy criteria are mainly administrative constraints or factors that need to be considered. For example, governments would like to be confident that a new policy initiative can be delivered without high administrative costs and that the lines of accountability for outcomes are clear. But a federal strategy for seniors’ care would not begin with an overriding objective of administrative efficiency or accountability. Economic efficiency, horizontal equity, mobility and political credit are other factors that would be considered in policy decisions but are unlikely to be overarching goals.34
But the four other criteria could also be policy goals. A federal government could well have as a goal increasing personal autonomy for seniors who require care. Or it might be concerned about the legacy of this generation to its grandchildren. In this case maintaining intergenera- tional equity could be a goal. If the government wishes to focus on people who are most in need, ensuring target efficiency and/or improving redistributive equity could be goals.
The next question is whether there are, among the eight options that do not raise federalism concerns, some that would advance these four goals. The answers are summarized in table 4. Personal autonomy is best supported by putting buying power into the hands of those who require care, rather than directing the same funds to provincial/territorial governments or NGOs. The reason is simply the old saw that “she who pays the piper calls the tune.” All five demand-side options meet that test. They would increase the financial capacity of seniors, which better enables them to pay for the care services of their choice. Supply-side options, to the extent that they increase caregiving capacity and the choices available, can also enhance personal autonomy, but they do so only in an indirect way. While option 7 is designed to sup- port informal caregivers by facilitating respite arrangements for them, it would operate mainly through the care recipient, and therefore it would also have direct personal autonomy benefits.
In the case of intergenerational equity, four of the five demand-side options would entail pre- funding and therefore would not add unfairly to the tax burden of younger people.35 Option 1 (OAS/GIS care supplement), however, is pay-as-you-go (PAYGO) and would increase the tax/debt burden on today’s workforce, especially the younger cohorts, and increasingly so as the population ages. Supply-side options that increase the number of care providers for today’s seniors would entail a transfer from today’s younger taxpayers (though seniors also pay taxes), while those that increase longer-term care capacity (for example, by building new assisted living facilities and training future caregivers) would probably also benefit them at some point in the future (option 9).
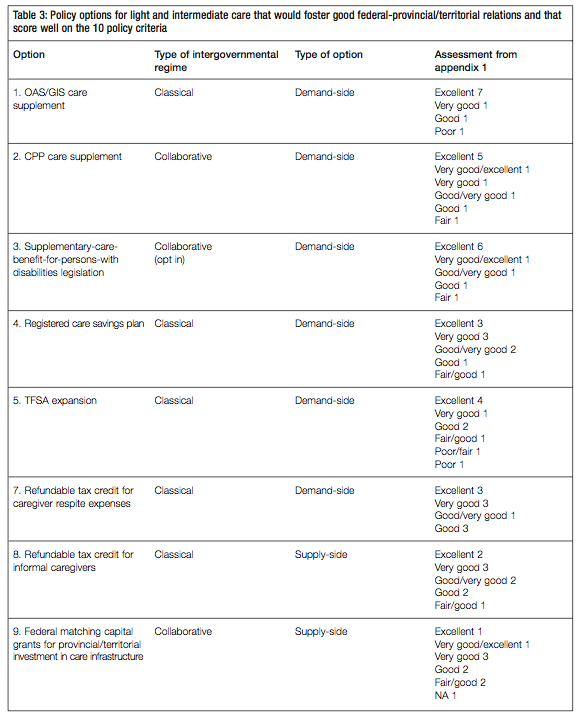
Target efficiency can be defined in several ways. Under a broad definition that aims to provide public resources where they may be needed, all the options would work. However, under a narrow definition that aims to ensure that money is spent exclusively on seniors’ care, only options 1, 2, 3, 4, 7, 8 and 9 would fit that bill.
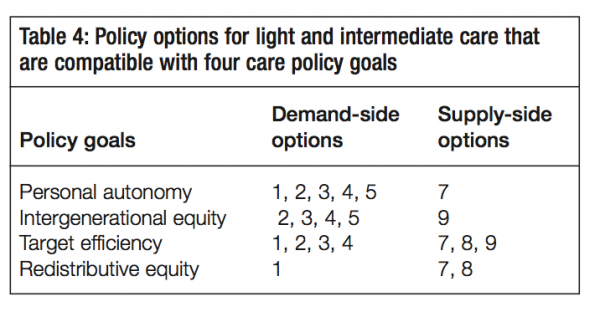
As for improving redistributive equity, options 1, 7 and 8 would achieve that goal by design, whereas option 2 and 3 could be used for that purpose by adjusting the contribution/benefit rate structure accordingly.
These points are captured in table 4. What is important to note here is that there are both demand- and supply-side policy options that are consistent with all four goals. These goals are sufficiently different from one another that some could appeal to a market-oriented con- servative government, others to a social democratic government and still others to a gov- ernment of the centre. In a nutshell, at the light and intermediate points on the care continuum there is a full range of policy initiatives available to the federal government that would be compatible with good intergovernmental relations and good public policy. For a federal government of almost any political stripe, therefore, there are opportunities to improve seniors’ care.
This section deals with policy options at the heavy end of the care continuum (table 5). As noted earlier, the considerations that apply here are substantially different than those that apply at other points on the continuum. The term “heavy” as used in the con- text of this study is not intended to replace the more conventional term “complex.”36 The type of care required at this end of the continuum is indeed complex, due to the presence of multiple disabilities and the need for professional supervision and personal assistance, sometimes around the clock. The term “heavy” is meant to convey the idea that most indi- viduals who spend an extended period of time in complex care incur costs that are beyond their financial reach. A person who receives complex care for six months and then dies has experienced a substantially different financial burden than a person who is in complex care for years.
The policy options to address light and intermediate care needs involve both the private and the public sectors. In this section, only public sector options are suggested. The reason is sim- ply that it is unrealistic to base policy on the expectation that individuals should and will be able to provide for themselves in the unlikely event that they need costly, complex care for a lengthy period of time at some point in their life. This would require that most people over- save to the point that they would have a much higher standard of living after retirement than they did in their working years.
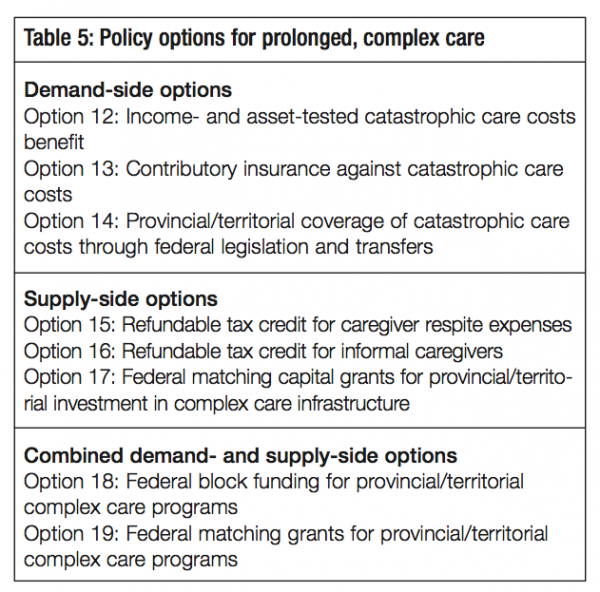
Social insurance is the way in which public policy deals with a situation where there is a relatively low probability of incurring high costs by pooling risk over a larger group. Social insurance is often defined as including only those programs in which all or the bulk of the funding is raised through mandatory ear- marked employer and employee contributions that are paid into a fund that is segregated from other government finances and from which benefits are paid. The definition adopt- ed here is broader. It includes any government program that spreads the risks of an uncertain future over all of the taxpaying public. This avoids a long discussion of exactly where the cut-off points are for the purposes of satisfying the more conventional definition.
There are many types of social insurance programs in Canada, each with its advantages and disad- vantages. Some programs, such as Employment Insurance (EI), are paid for through earmarked taxes and others, such as medicare, mainly through general revenues. Some are funded (the CPP and the QPP are partially funded), others are PAYGO (the OAS and the GIS). Social insurance can be provided through either income support or service programs. In the case of income support pro- grams, participants are entitled to benefits when certain contingencies materialize, as is the case with EI, Workers’ Compensation, the CPP, the QPP, the OAS and the GIS. Public health insurance is the largest service program in each province, and thus the largest in Canada. It is a social insurance program in the broad sense in that society covers the cost of medical, hospital and many diagnos- tic services, partly from provincial revenues and partly from federal revenues through the CHT.
Social insurance programs can operate at either the provincial/territorial level or the national level. A disadvantage of social insurance that is provincial rather than national is that it limits the size of population over which the pooling of risk occurs. This would be an important issue for the less populous jurisdictions in particular. Also, in the absence of a pan-Canadian pro- gram, regional differences in public coverage and access to care services could become a factor in seniors’ decisions about where to reside. This in turn could lead some provinces to impose residency requirements. In the case of seniors’ care, for instance, some provinces (notably British Columbia) are consistently net receivers of older migrants from other provinces and ter- ritories, while others are net “exporters.” Thus, there is a case to be made that all of Canada should be the sharing community for catastrophic care costs and, therefore, that Ottawa should assume a leadership role in shaping strategic policy to that effect.
A federally financed social insurance program for catastrophic care costs could be attractive to both orders of government. It would relieve the provinces/territories — sooner or later, depending on details of the program design — of the growing cost of subsidizing those seniors who have the greatest care needs. And it would do so without undermining the provinces/ territories’ exclusive authority to make laws relating to the protection of care recipients, the certification of care professionals, the approval of group residences and other care-related responsibilities. What might be appealing for Ottawa is the fact that this would entail a national project that addresses an important societal and fiscal challenge in an equitable (again, depending on the details), economically efficient and fiscally responsible fashion. The challenge in considering such options is whether they can be designed in a way that meets the insurance objective without sideswiping provincial/territorial care programs.
Three categories of demand-side options are discussed in this section, reflecting Canada’s diverse experience with different kinds of social insurance programs. The first two involve fed- eral transfer payments to persons incurring catastrophic care costs, one on a PAYGO basis and the other on a fully funded basis. The third category entails new services delivered by the provinces/territories on a PAYGO basis, with additional funding from Ottawa. Federal transfers to provinces and territories (block fund and matching grants) for operating expenses related to catastrophic care costs are also considered. Analogous to options 10 and 11 above, these trans- fers would leave it to the provinces and territories to decide whether to use the funds to sup- port the demand side, the supply side or both.
The demand-side options involve federal payments to and for seniors whose eligible expenses exceed some definition of catastrophic care costs.
This option would consist of a noncontributory benefit for persons who, after reaching age 65, incur cumulative care expenses that exceed a defined threshold of catastrophic costs. All eligible expenses beyond the established threshold would be paid for, although benefits would be income- and asset-tested. The benefit would be paid out of general revenues and provided as a refundable tax credit, which means it would also be available to those who do not have enough taxable income against which to offset the benefit. While this study does not include program design details, the data below give some idea of the range of care costs involved.
The costs of long-term care facilities for residents vary by province and depend on whether they are publicly subsidized or entirely privately paid and on the type of accommodation (standard, semiprivate or private). A 2009 study by the Canadian Union of Public Employees found that in publicly subsidized facilities the annual cost to residents ranged from roughly $12,000 to $36,000 (2009, 22). It also found that the average rent in unsubsi- dized for-profit private-pay facilities in six provinces ranged from $30,000 to $60,000 annu- ally, even though these facilities provided a lower level of care than the subsidized ones.37 Given that the median annual after-tax income of those aged 65 and over in 2007 was $21,300 for single women, $23,400 for single men and $44,900 for couples, it is clear that private facilities are beyond the means of a large majority of seniors. According to a study by the National Union of Public and General Employees, most provinces apply a means or asset test as well as an income test for the subsidies they provide for seniors’ care. In the Atlantic provinces and Quebec, “an individual must liquidate a percentage of the family’s assets, including savings and investments,” before they can receive a subsidy (2007, 18). The remaining provinces except Alberta employ an asset test, which excludes family assets.
All of this suggests that in most provinces many current long-term care residents have already liquidated at least some of their assets. Indeed, as a result of income tests, long-term care resi- dents in the four western provinces are typically left with a monthly income of $200 to $300, and considerably less in central and Atlantic Canada, to cover other expenses. It is also note- worthy that provincial governments and long-term care facilities often bump up their rates when residents receive pension increments. In a sense, therefore, the federal government is a party in a triangular financial relationship with elderly citizens and the provinces/territories, and this type of federal initiative would clearly intensify the dynamics of that relationship.
For the provinces/territories, a federal catastrophic care costs benefit would create an incentive to reduce if not eliminate subsidies to long-term care facilities and their residents. Whatever the federal threshold for defining catastrophic costs, the lower the provincial/territorial subsidy the sooner the federal program would be triggered. And ultimately, the lower the subsidy the greater the cost saving to provincial/territorial budgets. Indeed, a corollary of this option is that if the federal asset test is more stringent than the provinces’, the federal benefit might never be triggered for those long-term care residents with “excess” assets. As for long-term care residents and others with heavy care costs, if they could find a voice it would argue that provincial/territorial income and asset tests leave them with too little money to pay their other bills. They would seek to retain a share of the federal bene- fit. The government of Canada would also have interests. One of these would be to make sure that the provincial/territorial increases in the amounts charged to long-term care residents (the subsidy reductions) meet some test of reasonableness. Federal ministers might also want to ensure that at least some of the federal money stays with seniors in order to gain some political credit.
Under this option the federal government would have to decide which expenses are eligible. It would need to determine when the catastrophic care cost threshold has been reached and also to make clear which expenses it would pay for beyond that threshold. Eligible expenses would likely include other expenses in addition to those charged by long-term care facilities. Some persons do receive their care and incur their costs at home. Those who are in care facilities could have incurred eligible costs before they entered the facility. Also, there may well be non- insured health-related expenses.
Establishing federal eligibility rules raises issues about the interaction between the federal pro- gram and existing provincial/territorial care programs. The federal government could decide that its rules for establishing which categories of care expenses are eligible would parallel the rules that each jurisdiction uses for the purpose of determining eligibility for its own subsidy programs for care expenses. This would mean that the effective threshold for the federal bene- fit would differ from one jurisdiction to another, since subsidies differ from jurisdiction to jurisdiction. On the other hand, if Ottawa applies the same rules across the country, there would be two sets of rules within each province/territory, one for the purpose of determining if and when a person qualifies for the federal benefit and another for the purposes of provin- cial/territorial programming. This trade-off would not be easy to resolve.
The federal government has extensive experience in delivering income-tested programs and refundable credits, but not in asset testing. However, it does have some relevant experience, for example, in taxing estates and real estate gains. The assumption here is that for income- and asset-testing purposes it would be necessary for taxpayers whose care expenses exceed the threshold definition of catastrophic costs to provide income tax statements, including docu- mentation on financial and real assets.
As noted above, an advantage of this scheme for the provinces/territories would be that Ottawa would effectively absorb some of the costs that they now pay in their capacity as pay- ers of last resort. Would this advantage outweigh the complexity of having Ottawa engaged in overlapping programs that could have an impact on their own programs? If the result is two sets of rules in each jurisdiction, the provinces/territories might lose interest. In jurisdictions where the federal rate for eligible expenses is higher than the provincial/territorial rate (e.g., accepting as eligible expenses higher rates of pay for caregivers or higher rents in caregiving facilities), the provinces/territories might worry that formal caregivers and care facilities would try to lever rate increases from them, using the federal tariff schedule as a bargaining tool.
There appear to be two legislative routes for achieving the same outcome under this option. The first would entail amending the Old Age Security Act. Parliament would enact a supplement to the OAS/GIS for persons whose care expenses exceed some threshold. The second route would be through the income tax system and thus implicitly the spending power. Two questions arise in choosing between them. Is it more likely that a commitment made under the OAS Act would be shielded during one of Ottawa’s periodic expenditure reviews than a comparable commitment made under the Income Tax Act? Would the choice of legislative mechanism influence the willingness of the provinces and territories to coop- erate with Ottawa in making the catastrophic care costs benefit politically viable? Implicit in the second question is the judgment that this option would not be workable if it does not enjoy a degree of provincial/territorial support.
Whether it uses the Old Age Security Act or the Income Tax Act as its legislative tool, the federal government would need the support of at least a majority of the provinces/territories. This would be the case explicitly if the Old Age Security Act is employed, since a province would be able to exert its constitutional powers under section 94A to effectively override the federal program. If the same federal program is introduced under the Income Tax Act, the province could still block it by introducing legislation that would render it ineffective. But even apart from the legal considerations, the provinces/territories would almost certainly be able to dis- courage the federal initiative by refusing to cooperate in practical ways.
Consider a situation where, say, there is agreement from seven provinces with two-thirds of the population (the same as required for a CPP amendment), but only that degree of support. What would Ottawa do if the nonconsenting provinces passed legislation to keep it out? Assuming the federal government decides to proceed, this would mean that the federal benefit would not be available to residents in those three provinces, who, as federal taxpayers, would be effectively subsidizing the taxpayers in the other seven.
If the constitutional context were different, it might be appropriate for the federal gov- ernment to take a hard stance and state that it is proceeding with its program and that it looks forward to the day when the three opposing jurisdictions join in. But the fact that section 94A makes it clear that provinces have paramountcy in respect of old age pen- sions and supplementary benefits suggests that the Constitution does not anticipate Ottawa playing tough with the provinces on those items.
In general, opting out is used for programs that involve federal transfers to governments, not to individuals or organizations. But there is a precedent for opting out in the case of university grants (1960) and youth allowances (1964). It could be appropriate in this kind of situation to avoid the cross-subsidization between federal taxpayers in participating and nonparticipating jurisdictions.
This is also a social insurance option to protect the small percentage of the elderly population faced with catastrophic care costs. It would entail the creation of a new “catastrophic care costs benefit” (CCCB) that would be available to any participant who incurs, cumulatively after age 65, eligible care expenses that exceed a defined threshold of catastrophic costs.38
The CCCB threshold chosen would affect the cost of the program, but the assumption here is that it would be in the order of tens of thousands of dollars. Amounts of this magnitude are not out of line, given that in 2005 the median net worth of families aged 65 and over was in excess of $300,000, higher than for all other age groups, except those in the 55-to-64 age bracket (half of whom would be over 65 by now). It is difficult to argue that cumulative care costs in the $20,000-to-$30,000 range would be catastrophic for the one-half of families that are at or above the median, or even for those that are slightly below the median.
This option differs from option 12 in two ways. It would be prefunded, whereas option 12 is PAYGO. This means that CCCB payments would not begin for many years, whereas under option 12 payments could start soon after passage of the legislation. Also, the CCCB would become payable when the threshold for catastrophic costs has been reached, without the income and asset tests imposed under option 12. The tests would not be necessary, because the contingent benefit would be fully funded.
As with option 12, the two orders of government would need to decide which care expenses are eligible. If Ottawa adopts the provincial/territorial rules for eligible care expenses in each jurisdiction, the effective threshold for the CCCB would differ from one jurisdiction to anoth- er and coverage would differ after the threshold is reached. On the other hand, if Ottawa establishes national eligibility rules, there would be two sets of rules within each province/ter- ritory, one for determining if and when a person qualifies for the CCCB and another for provincial/territorial programming purposes. This trade-off would not be easy to resolve.
Two mechanisms are available to achieve this. The first is through an amendment to the CPP; the second entails a separate disability care statute.
The CPP already includes disability provisions, and there are federal administrators familiar with the issues related to disability. However, given the stringent CPP amendment rule, the diversity of economic and social conditions among the provinces and the range of ideological perspectives among provincial governments, this route would be difficult to navigate political- ly. There is also the issue of whether Quebec would be willing to amend the QPP Act along the same lines. This explains why CPP amendments are rare.
A premise in this case is that the CCCB would be available to a cohort only to the extent that it has paid for the benefit. This is to ensure that younger members of today’s workforce, and those who will join the workforce in the years to come, do not end up paying twice — for their own benefits and for a share of the benefits of today’s middle-aged and older workers. If this premise is accepted, there are a number of ways of designing the contribution/benefit structure, each with advantages and disadvantages.
The first alternative would be to require only those under a certain age — say, 30 — to con- tribute to and ultimately be eligible for this benefit. This would have the advantage of ensur- ing that younger generations do not subsidize their elders. The disadvantage would be that the benefit would not be available for another 35 years, which does not fit well with the demographic considerations that gave rise to this study.
A second alternative would be to require CPP plan members who are older than, say, 30 years of age to contribute at higher rates so that each cohort pays for the full costs of the benefit. This would avoid intergenerational subsidization and make the benefit available much sooner. However, the contribution rate increase for the oldest cohorts would be substantial (at least in relative terms), and it would also apply to employers with older workers.
A third alternative is a compromise between the first two, where all CPP plan members between the ages of, say, 30 and 55 would be required to participate on the basis of each cohort paying its own way. Under this alternative, CPP participants over the age of 55 would not be eligible to participate and therefore would not have to contribute.
There are obviously many other design possibilities, all with their own trade-offs. Once the program matures, it would displace some of the subsidies that the provinces/territo- ries pay to or on behalf of complex care patients who are unable to pay for the services.
The second mechanism is a funded catastrophic care costs benefit implemented through a “seniors disability care act.” Section 94A of the Constitution authorizes Parliament to enact laws relating to old age pensions and “supplementary benefits, including survivors’ and dis- ability benefits irrespective of age.” Technically, it could do so without the agreement of the provinces. But since section 94A also states that no such federal law shall “affect the operation of any law present or future of a provincial legislature in relation to any such matter,” a province could effectively prohibit the implementation of a new federal program within its jurisdiction. One or more provinces might wish to do so for any of several reasons: opposition to a new federal earmarked tax on taxpayers in its jurisdiction; inconsistency with the spirit of the consensus provisions of the CPP; overlap with provincial programs leading to confusion and waste; or symbolic considerations (opposition to Ottawa intervening through legislation where the province has primacy).
The basic design of the benefit would be the same as under option 13a. Ottawa might choose this alternative if it is unable to obtain sufficient provincial support to meet the CPP amendment rules. If all or almost all provinces are opposed, the politics of Ottawa legislat- ing new statute law might be very difficult. But if, for the sake of argument, five or six provinces, with well over half the population, favour the substantive proposal outlined in option 13a, then option 13b might be a solution for all jurisdictions. Parliament would enact the new law under section 94A. The opt-in, opt-out choice and consequences would be the same here as in option 3.
If Quebec concurs, it would have three choices. It could do nothing, in which case the federal law would apply in Quebec. It could pass parallel legislation, or it could amend the QPP. Amending the QPP is the most likely approach, and allowing the federal law to apply the least likely. The eligibili- ty rules issue would not arise for the QPP amendment, because the Quebec government would be the decision-making authority for programs related to both catastrophic and non- catastrophic care expenses.
The third broad approach to catastrophic care costs involves legislation to insure publicly those care services that currently are not covered. Option 14 would provide coverage for the necessary care expenses that exceed a defined threshold of catastrophic costs. It would require agreement between the two orders of government. To secure the support of the provinces/ter- ritories for such an agreement, the federal government would have to transfer more financial resources to them than it does today. This incremental transfer could take the form of a new grant program, but the provinces/territories would likely prefer to have the incremental cash transfer added to the Canada Health Transfer, since it affords them more flexibility.
The benefits provided under this option would be similar to those under option 12, but not identical. As in option 12, what constitutes catastrophic care costs would have to be deter- mined. One important difference is that in this case the provinces would deliver the benefits (through services/subsidies provided to care recipients), whereas under option 12 Ottawa would provide a cash benefit directly to care recipients. Another difference is that under option 12 federal authorities would be able to specify all the design features of the program. Option 12 would impose few if any legal constraints on Ottawa, since it would be enacted under a constitutional power (section 94A) that authorizes the federal government to make laws. But option 14 relies on the spending power for its constitutional authority. This authori- ty would enable Ottawa to require that a province or territory provide certain broad categories of care support as a condition of funding. But it would preclude Ottawa from specifying all the program parameters.
Again, two mechanisms are available. One would be an amendment to the Canada Health Act (CHA) to extend the scope of its coverage to include catastrophic care costs. Another would be to enact a new statute similar to but separate from the CHA. In either case, these new commitments would require bilateral agreements with the provinces and territories. If Ottawa offered to pay all or a significant portion of the related costs, the provinces/territories would see their costs reduced.
For some time there have been calls to extend the scope of the CHA to include uncovered health care costs. The catastrophic care costs benefit proposed under option 12 would be income-tested through either the Income Tax Act or the OAS Act. Indeed, OAS benefits are already income-tested. But under the CHA as it now exists, there is no provision for income or asset testing. And a proposal to amend the CHA to cover catastrophic care expenses on an income- or asset-tested basis would almost certainly raise concerns that such an amend- ment would create an unfortunate precedent for the CHA. The argument would be that such an amendment would create a slippery slope that might one day weaken the universality of the hospital, diagnostic and medical services that the CHA now covers.
During the post-Second World War discussions on public health insurance, the federal and provincial governments did not commit to universal publicly insured hospital and medical services until they were satisfied that the supply was adequate to meet the anticipated growth in demand. There are now severe caregiver shortages, and there appear to be shortages of long-term care beds in nonhospital institutions as well. If this option is pursued, the supply side would have to be ramped up.
Another issue is whether the federal law would enable the provinces/territories to use different definitions of “catastrophic” care expenses in the same way that each province was free to define the “persons in need” provision under CAP. Some differences would be logical, given the differences in socio-economic circumstances among the jurisdictions.
This option addresses two concerns. First, the federal government might consider that having definitions of catastrophic care costs that vary from one jurisdiction to another is fitting and desirable, given the disparities in real incomes and asset allocation among the provinces/territories. This in turn leads to the argument that these new benefits should not be included as part of the CHA, since jurisdictional differences in coverage are not compatible with the some of the Act’s principles and this could set an undesirable prece- dent. Second, with this option the federal government could avoid opening up the CHA if it is concerned that this would trigger a debate on other unrelated aspects of the Act.
Accordingly, option 14b is the same as 14a in that it would require agreement on the amount of money that Ottawa would transfer to provinces and territories for this purpose, and it would be the provinces/territories that would administer the program. Under this option, however, Parliament would enact new statute law, a “seniors disability care act,” in order to set this program apart from the CHA.
According to the Canadian Institute for Health Information (2010), the majority (98 percent) of seniors aged 65 and older receiving publicly funded long-term home care services have one or more informal caregivers. Thus, even though in complex care cases the role for formal care is relatively more important, informal care is often an essential component. Accordingly, options 7 and 8 also apply at this end of the care continuum.
This is similar to option 7. However, the fact that in the cases of prolonged, complex care a higher proportion of caregivers would likely be assisting individuals who have severe impairments raises questions as to whether this option would be practical or effective for care recipients who are not able to make use of the tax credit without the help of a desig- nated person. Alternative mechanisms for funding respite for informal caregivers might also be needed as a fallback.
This is the same as option 8, but the case for supporting the informal caregivers of individu- als requiring prolonged, complex care is even stronger than it is for helping those providing lighter and intermediate care. Some provinces have already begun to use this approach. It will be recalled that in its first phase this option would be based on pilot projects to deter- mine the appropriate design and level of incentive. Given Canada’s demographics, the parameters of this program would have to be assessed carefully in order to minimize unde- sired labour market effects.
This option is identical to option 9, except that the capital investment would be focused exclusively on enhancing the supply of skilled caregivers and specialized facilities required by individuals in complex care. As the first cohort of baby boomers will enter their 80s in 15 years (2026), this option should be given serious consideration.
The federal transfers to the provinces/territories proposed under the next two options are intended to cover their operating costs related to complex care. Each jurisdiction would decide how much of this new funding would be used to subsidize more clients, thus sup- porting the demand side, and how much would go to hire more caregivers or invest in the training of existing caregivers, thus enhancing supply.39
This is similar to option 10, but its specific purpose would be to help the jurisdiction cover its operating costs in respect of subsidies or services provided to patients whose care costs have exceeded some defined threshold. It is thus more targeted than option 10. But like option 10, it would rely on the spending power for its constitutional authority and it would raise the same questions about how to define base-year operating costs and how to determine the amount of transfer in year 1 and its annual rate of growth.
If, as a condition for this transfer, Ottawa requires that all jurisdictions use the same defini- tion of catastrophic costs and eligible care expenses, it might be necessary for each province/territory to draw up two eligible expense schedules — one for its own programs and one for the joint program with the federal government. The provinces/territories would likely resist. Moreover, to make such a detailed regulatory scheme a condition of the trans- fer might exceed federal constitutional authority. The most likely outcome therefore is that provinces would accept a general obligation to cover catastrophic care costs, with each hav- ing the legal discretion to do so subject to some de minimis rule. As noted for option 14a, the precedent might be the shared-cost arrangements under CAP, whereby each province had its own definition of “person in need” and the definitions varied considerably.
This is similar to option 11, but the matching grant would be for incremental catastrophic care costs only. The difficulty in establishing the relevant base-year-per-capita amount for provincial/territorial expenditures would arise here, as it would in option 18. The same trade-off related to federal eligibility rules for care expenses would apply here. Under this option, however, the trade-off would be less difficult than under other options, since the provinces/territories would be cost-sharing, which means there would be a strong case for using provincial/territorial rules and definitions. Since this would be a matching grant, it is assumed that Ottawa would put a cap on federal outlays.
Figure 4 illustrates the kind of federalism that is implicit in options 12 to 19. It is worth repeating that options below the horizontal axis would normally not cause major distur- bances in the federation. Option 13 (contributory insurance against catastrophic care costs) is shown close to the bottom of the vertical (hierarchical/nonhierarchical) axis. Since options 13a and 13b would entail roughly the same degree of interdependence and non- hierarchy, they are not shown separately. Option 13a would require a CPP amendment and therefore significant collaboration between the two orders of government. And option 13b, with its opt-in, opt-out provisions, is premised on the assumption that no province should be coerced into accept- ing a program that it does not support. Neither option would be coercive and both would require intergovernmental collaboration.
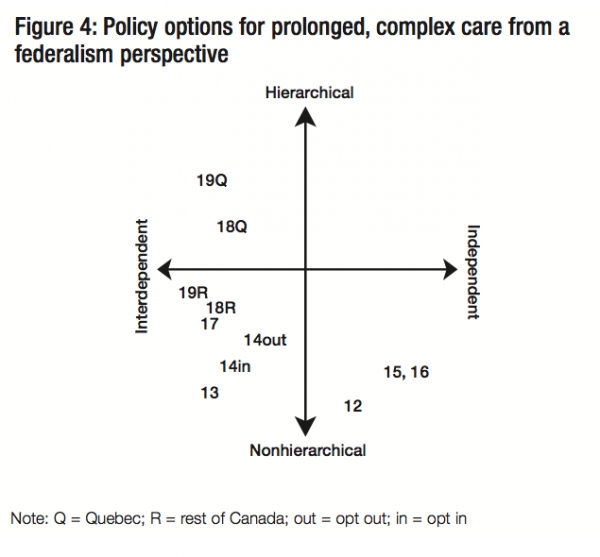
Option 12 (income- and asset-tested cata- strophic care costs benefit) is in the classi- cal federalism quadrant because such an initiative would be within federal consti- tutional jurisdiction, whether the mecha- nism used is the OAS Act or new disability legislation. Provinces also have constitutional authority, however. Accordingly, to the extent that Ottawa’s definition of eligible care expenses differs from those of individual provinces and territories, there would be the risk that this federal initiative would compli- cate the administration of their care programs. It is for this reason that this option is posi- tioned closer to the midpoint of the independence-interdependence horizontal axis than option 1, as shown in figure 3. Option 12 is also shown close to the bottom of the vertical (hierarchical/nonhierarchical) axis because its opt-out provisions would remove any sense that Ottawa is being coercive.
Option 14 (provincial/territorial coverage of catastrophic care costs through federal legisla- tion and transfers) is in the collaborative quadrant because it would involve both orders of government in an interdependent relationship. The provinces/territories deliver health care programs. The broad parameters of these programs have been shaped by many years of intergovernmental negotiation. The programs are paid for mainly by the provinces/terri- tories. Ottawa’s current share of funding is 20 percent if federal cash only is considered, and 30 percent if cash and the 1977 tax transfer are included. Option 14 is located higher up on the vertical axis than option 13. The reason is that Ottawa can amend the CHA and enact new disability legislation without provincial concurrence, whereas amending the CPP requires an act of Parliament and consensus of the provinces.
Option 14 would require extensive intergovernmental negotiations, however. To include catastrophic care costs under either the CHA or a new seniors’ disability care act, Ottawa would have to persuade the provinces/territories to cover such costs as a matter of entitle- ment, as they have done for hospital and medical expenditures for about 50 years. To secure the agreement of the provinces/territories, the federal government would have to make it worth their while financially. A key difference between options 14 and 18 (federal block funding for provincial/territorial complex care programs) is that under the former the provinces/territories would have to commit to cover all the catastrophic care costs of every senior, whereas under the latter they would use the federal transfer to improve the situation of seniors with catastrophic care costs, but they would not be obliged to pay all or any costs incurred by a specific person. In other words, option 14 would create an entitlement, whereas option 18 would not.
Option 17 (federal matching capital grants for provincial/territorial investment in complex care infrastructure) is comparable to option 9. Although it would entail use of the federal spending power, the grants would be time-limited and focused on capital costs. Therefore this option should not raise serious intergovernmental problems. In figure 4 options 18 and 19 (federal block funding and federal matching grants for provincial/territorial complex care pro- grams) are placed in the same position as options 10 and 11 are in figure 3.
Appendix 2 provides a summary assessment of options 12 to 19 using the same 10 policy criteria that were used to evaluate options 1 to 11. Several of the points made above in the analysis of light- and intermediate-care options also apply to options at this end of the care continuum.
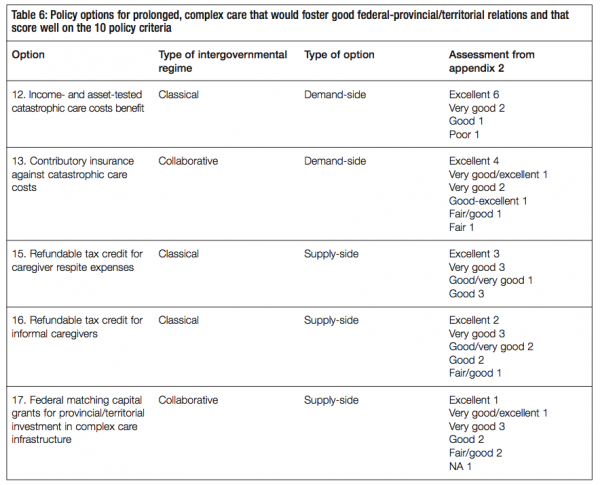
First, the options that raise few concerns from a federalism perspective are also strong from a policy perspective. Second, there are policy options on both the demand and the supply sides that are compatible with those criteria that could serve as policy goals. These results are sum- marized in table 6. Third, the scope of potential options is broad, with ideas that could appeal to governments of different political orientations, whether market-oriented conservative, cen- trist or social democratic. Given these similar results, the focus here will be on the similarities and differences among the options for prolonged, complex care.
As was the case with options for light and intermediate care, the demand-side options for pro- longed, complex care also performed well based on policy criteria. Options 12 and 13 (income- and asset-tested catastrophic care costs benefit, and contributory insurance against catastrophic care costs) were assessed much more favourably than option 14 (provincial/terri- torial coverage of catastrophic care costs through federal legislation and transfers). The princi- pal reason is that option 14 would entail intergovernmental transfers, whereas options 12 and 13 would provide benefits directly to individuals who qualify. As a result, option 14 did less well on criteria such as accountability, political credit and administrative efficiency.
The supply-side options 15 to 17 also performed well. The two options that would involve federal conditional sharing of operating costs did not fare nearly as well. Option 18 (federal block funding for provincial/territorial complex care programs) and option 19 (federal match- ing grants for provincial/territorial complex care programs) were evaluated as “fair” or “poor” on four of the ten criteria.
Under options 12 and 13, extensive federal-provincial/territorial consultation would be necessary to define catastrophic costs and eligible expenses. The issue of whether to have one or two rate schedules for caregivers and caregiving institutions in each jurisdiction would need to be resolved. For option 13a, the complexities of achieving the necessary fed- eral-provincial/territorial consensus required for a CPP amendment and the desirability of a deal with Quebec to maintain parallelism between the CPP and the QPP would constitute a big hurdle. There would be less of a hurdle under option 12, because Parliament has the authority to legislate without the approval of the provinces/territories. In reality, however, Ottawa would be unwise to act without the provinces’ agreement, since this could increase the risk of administrative snafus and could damage intergovernmental relations.
None of these considerations means that the two options should be put on the policy back burner. While Canadians may be facing a period in which fiscal resources are tight, there is never a good time as there are always more claims on the public purse than can be satisfied. In any case, the issues surrounding seniors’ care entail medium- and long-term planning horizons that extend well beyond the next 12 to 18 months. The federal government could, for instance, choose to act on one of the options, undertake whatever intergovernmental negotiations are needed, introduce the required legislation in Parliament and secure its enactment, but plan to bring it into force only some years into the future. If the govern- ment waits for the right time to legislate, it may wait forever.
If the federal government thinks that option 12 is a good long-term strategy, or if it reaches an agreement with provinces regarding option 14, the situation would be somewhat analo- gous to the one at the end of the Second World War in relation to health insurance. At that time Ottawa tried to convince the provinces to join in a national health insurance scheme. Several provinces, including the two largest, balked. It took another two decades before both universal hospital insurance and medical insurance became available on a Canada-wide basis.
However, even if all the provinces had agreed in 1945, the existing capacity of the health system (e.g., the number of health professionals and the physical infrastructure) would not have been adequate to deal with the ensuing growth in demand. The supply-side defi- ciency was recognized, and in the aftermath of its initial failure to muster provincial con- sensus on public health insurance, Ottawa created the National Health Grants Program. Launched in 1948, this capital grants program involved federal cost-sharing with the provinces in a major expansion of the health care system. Thus, when universal hospital insurance and medical insurance became realities on a country-wide basis in the late 1950s and mid-1960s, respectively, adequate levels of skilled health care personnel and physical capital were available to respond to the additional demand. In much the same way, if option 12 or option 14 were implemented tomorrow, it is doubtful that current human resources or infrastructure would be sufficient to cope.
There is currently a significant gap between demand and supply in seniors’ care services, and the federal and provincial governments (some more than others) have taken steps over the last several years to begin to address the shortfall. These actions suggest that there is a growing awareness in government circles of the challenges that Canada will face with respect to care for seniors over the next couple of decades. They do not, however, demon- strate awareness of the magnitude of the challenges. Most new public programs, including federal programs, barely qualify as baby steps. In order to gain the necessary perspective, governments should examine available empirical evidence and quantify the current gap. With that benchmark as a starting point, they need to estimate the extent to which this gap might be expected to grow over coming decades under current policies. Given current demographic and epidemiological knowledge, this task is doable. Statistics Canada has already researched many of the key variables (Carrière et al. 2008), and various groups have made similar projections for their particular purposes (Alzheimer Society 2010, 16-21).
While the demand-side options for light and intermediate care presented here include a role for the private sector, the options for prolonged, complex care do not. This reflects the argument presented earlier that pooling risk on the largest possible population base is the appropriate way to deal with the low risks and high costs associated with prolonged, complex care. With public-sector options, the issue of intergenerational equity must be considered seriously, as some programs could result in an unfair transfer of tax burden onto young and future workers. But there are options that would mitigate the risk. For example, option 13 is a contributory fund to cover future care costs, which would ease the tax burden on future generations. Option 17 would entail current taxpayers investing in current and future complex care capacity. Option 16 features pilot projects to test the effects of alternative tax incentives on the supply of informal caregivers, which could potentially reduce the need for more expensive formal care.
Earlier in this study I stressed the importance of personal autonomy. For people incurring considerable costs for complex care who still have the potential for a reasonable quality of life, the fact that all three demand-side options would put more money in their hands to purchase care services and meet other needs should increase their personal autonomy. Under options 12 and 13, the federal government would pay benefits directly to those eli- gible, whereas under option 14 Ottawa would transfer money to provinces and territories for the same purpose.
While personal autonomy would remain a priority for some patients, factors like pain man- agement, patient safety and end-of-life situations loom large for those who require pro- longed, complex care. These considerations speak more to the supply side than to the demand side. Option 17 is a supply-side measure that is based on the precedent of the National Health Grants Program, which helped develop the health care system after the Second World War. In the coming decade, that option could be used to ensure that there is an adequate supply of trained professionals and long-term care facilities to manage the anticipated growth in the population requiring complex care. While this would require a series of agreements between the two orders of government, the provinces/territories have much more to gain than to lose in such arrangements.
The analysis here suggests that demand- and supply-side options are not substitutes for one another but are complementary. Ideally they should be implemented sequentially, with the supply-side options dealt with first. Timing would be an important factor to con- sider. For instance, if there is federal-provincial/territorial agreement on option 13, benefits would not become payable for some years into the future, although how many years would depend on design details. However, if option 12 is preferred, it should not be promulgated into force until there is an adequate supply of formal caregivers and the appropriate physi- cal infrastructure is in place.
The array of federal policy options for prolonged, complex care is not as large as it is for light and intermediate care. But it is wide enough to present the federal government with opportunities to play a constructive role on the demand side, the supply side or both. Unlike the options presented for the light and intermediate points on the care continu- um, the options for prolonged, complex care do not contemplate “go it alone” alterna- tives. On both the demand side and the supply side, all the options are premised on the need for genuine intergovernmental collaboration.
The fact that demographic trends are causing the aging of Canada’s population has been known for decades. Yet Canada does not have an overarching policy strategy to deal with the costs and opportunities embedded in the aging process.40 Nor does it have a national policy for dealing with the effects of aging on the demand for and supply of care.
The constitutional responsibility for care rests with provincial governments. Although each province and territory is responsible for what happens within its borders, these jurisdictions do not have joint responsibility for the country as a whole. The federal government is the logical body to provide countrywide strategic policy direction in regard to aging and its effects on care, provided that it does so in a manner that respects provincial jurisdictional and legislative competence.
What Ottawa should do and how it should be done, however, is not an academic exer- cise. They depend on the facts on the ground. This study is premised on the current imbalance between the demand for and supply of care for seniors and the expectation that this imbalance will grow. The exact size of the imbalance or its trajectory over time is not known. Therefore, as a first step toward clarifying what its role could and should be, the federal government must gain a better grasp of the demand-supply relationship.
Despite the lack of clarity on what its role should be, the federal government has over the years used both its constitutional heads of power (pensions, unemployment insurance, tax law) and its spending power (transfers to provinces) to make laws and allocate resources that have, intentionally or otherwise, influenced the demand for care and also, to a much lesser extent, affected its supply. The most significant policies, implemented by both the Liberals and the Conservatives, have been those pertaining to retirement income. Neither party, however, has explicitly made the connection between the outcomes of these policies and the demand side of the care market. As for the supply side, both parties have implemented several small measures such as tax breaks or direct grants that were explicitly aimed at caregivers or care recipients. But these constitute tinkering at the margins. They were introduced without undertaking a comprehensive analysis of the problem, or of the role the measures were meant to play in the solution. They were more about politics than about policy.
The Liberals under Jean ChreÌtien and Paul Martin had the opportunity to do more. Budget 2000 and the following fiscal update proclaimed victory on the deficit and noted that the federal debt was falling and the unemployment rate was at a 20-year low. This provided a window of opportunity to do something big. It could have been about aging, but as things turned out, it was about tax relief — a cut of $100 billion over five years. A second window opened in 2003 and 2004 when the first ministers met to discuss health care reform. Depending on how one counts them, around 10 health care issues were addressed in the 10-year Plan to Strengthen Health Care. Not one of these issues was directed at aging. As the Liberals were defeated less than 18 months after the 2004 Health Accord, this failed opportunity may not have mattered. But a re-elected Martin government might have attached a greater priority to the aging issue and the seniors’ care file. Indeed, only a few months earlier the Liberal general election platform had stated the Liberals’ intention to “work with the provinces and stakeholder groups to develop a comprehensive strategy to increase support for ‘informal’ caregivers — spouses, children and close relatives and friends” (Liberal Party of Canada 2004).
This pattern of small, ad hoc initiatives has continued under Stephen Harper’s govern- ment. The 2011 federal budget included a nonrefundable caregiver tax credit with a maximum annual value of $300. It also removed the $10,000 cap on the amount that caregivers can claim in medical and disability-related expenses for an aging parent, sib- ling or other financially dependent relative. For most caregivers, the amounts involved are of no consequence. In some sense, these measures can be viewed as a symbolic ges- ture of support toward the beneficiaries. The 2011 budget also increased the Guaranteed Income Supplement by up to $600 annually for singles and $840 for couples. The budget did not link the GIS increases to care costs, but nonetheless this additional income enables eligible seniors to pay for more care services (unless provinces appropriate some of the benefit increases, which they could do since many provincial care programs are income-tested). To date the Conservatives have shown as little concern for the implica- tions of population aging as the Liberals.
The concern that motivates this study is that the federal government’s inaction on this file may help turn the tsunami of aging into a “perfect storm.” The coming of this tidal wave has long been forecast. This should have allowed the federal government sufficient time to plan for and manage its consequences. If the federal government has a plan, however, it has not made it public. If the government has reason to believe that Canadians will be able to cope with the aging of the population with only small “one-off” policy adjustments every now and then, it must share its analysis with the public.
What the public does know is that the proportion of the population aged 65 and over is projected to increase from 14 percent in 2009 to 23-25 percent in 2036, while the working- age proportion of the population is expected to decline from 69 percent to 60 percent over the same period. Under Statistics Canada’s medium-growth scenario, the popula- tion aged 80 years and over will be 2.6 times higher in 2036 than in 2009, and 3.9 times higher by 2061 (Statistics Canada 2011). Population aging is expected to greatly increase the prevalence of dementia in Canada. In 2008, 7 percent of Canadians over the age of 60 and 49 percent of those over the age of 90 suffered from dementia. According the Alzheimer Society, “by 2038 the number of Canadians (of all ages) with dementia will increase to 2.3 times the 2008 level, i.e., to 1.1 million people, represent- ing 2.8% of the Canadian population” (2010, 17). The costs of caring for a person with advanced dementia are high. Whether these facts and projections will eventually trans- late into widespread social distress is not known, but they do raise questions that the federal government should be able to answer.
The next opportunity to make meaningful policy decisions on aging and care will be in the context of the renegotiation of the major social transfers (the Canada Social Transfer and the Canada Health Transfer). The statutory authority for these payments ends March 31, 2014. One question the Harper government should now be facing is whether it wishes to use the renegotiation as an opportunity to act strategically on the aging file.
Although there are a number of initiatives that could qualify as strategic, there are two elements that are essential to the federal government’s positioning on this issue. First, it must make a diagnosis of how well the care needs of seniors are being satisfied today, and provide realistic projections of those needs at least a couple of decades into the future. Second, it must indicate what role Ottawa wishes to play going forward. In so doing, it will signal to other actors how the federal government interprets the challenges that lie ahead and what is expected of them — individuals, the family unit, friends and neighbours, business, the social economy, as well as provincial and territorial govern- ments. If the federal government accomplishes only these two things, there will at least be a basis for consultation with the public and discussions with the provinces and terri- tories about what needs to be done and who should do it. If it doesn’t do these things, this will suggest to Canadians that the federal government believes there is no major care problem lurking down the road.
In elaborating what its future role in addressing seniors’ care needs might be, the federal government should consider whether it is appropriate to continue to focus almost entirely on the demand side or whether it sees a larger role for itself on the supply side as well. The government could also indicate whether it proposes to be involved on the entire care con- tinuum or whether it considers that it has a comparative advantage in some parts of the continuum relative to others. It could go farther still and, after holding consultations with the public and the provinces/territories, announce the specific programs it proposes to act on and over what period of time.
Given current fiscal conditions and the degree of uncertainty in the global economy, the Department of Finance will almost certainly resist substantial new expenditure commit- ments by the federal government. Assuming it succeeds, this would not be a reason to avoid making a diagnosis or to defer elaborating a strategy. Indeed, if anything, the oppo- site is true. If there are large and growing unmet care needs and the federal government, for whatever reasons, does not consider it has a role to play financially in addressing these needs, it has a political and moral obligation to say so publicly. It is worth reiterat- ing that the federal government has no policy on seniors’ care. Even with the measures announced in the June 2011 federal budget, an amount equal to perhaps 2 percent of total federal retirement-related outlays (pensions, tax deductions and shelters in pension and registered savings vehicles) is targeted explicitly for seniors’ care and caregivers.
The federal government has had decades to prepare for an aging society. To their credit, Ottawa and the provinces have done much to improve Canada’s retirement income sys- tem during this period. And they also appear to be responding to evidence of growing problems related to declining pension coverage and income security within that system. In doing so they can make use of models that project how well current cohorts of working age population will fare when they retire in relation to both antipoverty standards and preretirement income. But here is the rub. These models do not contain basic information about the costs of care and its incidence. Ottawa must ensure that this gap is filled both to better evaluate the adequacy of pension policy and as essential input for determining its seniors’ care policy going forward.
The Constitution precludes Ottawa from regulating caregiving institutions, establishing standards for different caregiver occupations or certifying that occupational standards have been met. The federal government is not in the business of delivering care services directly to Canadians, except those for whom it has special responsibilities (the Canadian Forces and some Aboriginal people). This still leaves Ottawa with many choic- es regarding its role in seniors’ care going forward. The object of this study has been to encourage public debate and intergovernmental discussions about what the federal role should be. I have argued that the federal government has had a big impact on the demand side of care services, even when federal policies were not explicitly crafted for that purpose. My analysis has also shown that there is a range of policy instruments available to the federal government that are federalism-friendly (they respect provincial constitutional authority) and that meet other tests of good public policy. These instru- ments relate to seniors’ care needs across the care continuum on both the supply and the demand sides.
The range of policy instruments includes some that emphasize individual responsibility and markets and others that emphasize collective responsibility and the state. In the case of individuals and markets, there are some options that give priority to personal autonomy and choice, and others that narrow choice to ensure that funds intended for care are used for that purpose. Where the state is concerned, there are options that involve pay-as-you-go funding and others that involve prefunding. The issues of personal autonomy and intergenerational fairness are major factors that must be weighed in considering all the options. All political parties should be able to find some instruments and options that are consistent with their values.
There are many degrees of freedom for the federal government to show leadership in sen- iors’ care. Denying the responsibility to exercise this freedom would be one degree of free- dom too many.
Alberta. 1978a. Harmony in Diversity: A New Federalism for Canada. Alberta Government Position Paper on Constitutional Change. Edmonton: Government of Alberta.
—————–. 1978b. Department of Federal and Intergovernmental Relations. Fourth Annual Report, to March 31, 1977. Edmonton: Department of Federal and Intergovernmental Relations.
Alzheimer Society. 2010. Rising Tide: The Impact of Dementia on Canadian Society. Alzheimer Society of Canada. Accessed November 1, 2011. https://www.alzheimer.ca/english/ rising_tide/rising_tide_summary.htm
Baldwin, Bob. 2010. Pension Reform in Canada: A Guide to Fixing Our Futures Again. IRPP Study 13. Montreal: Institute for Research on Public Policy.
British Columbia. 2010. Ministry of Health Services. “The Facts on Senior Care in B.C.” For the Record. Accessed June 28, 2011. https://www.gov.bc.ca/fortherecord/seniorscare/ se_healthcare.html?src=/healthcare/se_healthcare.html
Canada Revenue Agency. 2011. “Registered Disability Savings Plan.” Ottawa: Canada Revenue Agency. Accessed November 11, 2011. https://www.cra-arc.gc.ca/E/pub/tg/rc4460/ rc4460-10e.pdf
Canadian Centre for Elder Law. 2010. “Chapter Five — Indirect Compensation of Caregivers through the Tax System.” Study Paper on Family Caregiving. Accessed June 28, 2011. https://www.bcli.org/ccel/projects/family-caregiving/ chapter5#III
Canadian Healthcare Association. 2009. “New Directions for Facility-Based Long-Term Care.” Policy Brief. Ottawa: Canadian Healthcare Association.
Canadian Institute for Health Information (CIHI). 2010. “Supporting Informal Caregivers — The Heart of Home Care.” Analysis in Brief, Health System Performance.
Canadian Life and Health Insurance Association (CLHIA). 2011. “The Vital Social and Economic Role of Canada’s Life and Health Insurance Industry – A Keynote Address by George Mohasci, President and Chief Executive Officer, Foresters.” Presentation to the Economic Club of Canada, Toronto, September 7, 2011.
Canadian Medical Association. 2010. Health Care Transformation in Canada. Ottawa: CMA.
Canadian Union of Public Employees. 2009. “Residential Long- Term Care in Canada: Our Vision for Better Seniors’ Care.” Ottawa: 2009.
Carrière, Y., J. Keefe, J. Légaré, X. Lin, and G. Rowe. 2007. “Population Aging and Immediate Family Composition: Implications for Future Home Care Services.” Genus 63 (1-2): 11-31.
Carrière, Y., J. Keefe, J. Légaré, X. Lin, G. Rowe, L. Martel, and S. Rajbhandary. 2008. Projecting the Future Availability of the Informal Support Network of the Elderly Population and Assessing Its Impact on Home Care Services, December. Statistics Canada Research Paper/Demographic Documents, catalogue no. 91 F0015M-no.009. Ottawa: Statistics Canada. Accessed February 16, 2011. https://dsp-psd.pwgsc.gc.ca/collection_2009/ statcan/91F0015M/9 1f0015m2008009-eng.pdf
CIHI (see Canadian Institute for Health Information).
CLHIA (see Canadian Life and Health Insurance Association).
Commission on the Future of Health Care in Canada. 2002. Building on Values: The Future of Health Care in Canada. Ottawa: Commission on the Future of Health Care in Canada.
Conservative Party. 2011. “Here for Canada: Stephen Harper’s Low-Tax Plan for Jobs and Economic Growth.” Accessed 31 October, 2011. https://www.conservative.ca/policy/ platform_2011
Council of the Federation. 2009. “Premiers Agree on EI Reforms and Call for a Retirement Income Summit.” Press release, Regina, August 6.
Ferley, P., N. Janzen, and D. Onyett-Jeffries. 2010. RRSP Contributions 1968 to 2008…and Beyond to 2020. Toronto: Royal Bank of Canada. Accessed January 12, 2010. https://www.rbc.com/economics/market/pdf/RRSP.pdf
Finance Canada. 2009. Tax Expenditures and Evaluations 2009. Accessed February 9, 2010. https://www.fin.gc.ca/ taxexp-depfisc/2009/taxexp09-eng.asp
Finance Canada. 2011. The Next Phase Of Canada’s Economic Action Plan : A Low-Tax Plan For Jobs and Growth. June 6. Accessed October 17, 2011. https://www.budget.gc.ca/ 2011/plan/Budget2011-eng.pdf
Fortin, S., A. Noël, and F. St-Hilaire. 2003. Forging the Canadian Social Union: SUFA and Beyond. Montreal: Institute for Research on Public Policy.
Grignon, M. Forthcoming. “Financing Long Term Care in Canada.” IRPP Study. Montreal: Institute for Research on Public Policy.
Health Council of Canada. 2007. Health Care Renewal in Canada: Measuring Up? Third annual report to Canadians. https://www.healthcouncilcanada.ca/en/index.php
Horner, K. 2011. A New Pension Plan for Canadians: Assessing the Options. IRPP Study 18. Montreal: Institute for Research on Public Policy.
House of Commons. 2008. Report of the Standing Committee on Health, Chair Joy Smith. Statutory Parliamentary Review of the 10-Year Plan to Strengthen Health Care. Accessed September 14, 2011. https://www.parl.gc.ca/House Publications/Publication.aspx?DocId=3577300&Language= E &Mode=1&Parl=39&Ses=2
HRSDC (see Human Resources and Skills Development Canada).
Human Resources and Skills Development Canada (HRSDC). 2009. New Horizons for Seniors Program Update. Ottawa: HRSDC. Accessed December 13, 2011. https://www.hrsdc.gc.ca/eng/ community_partnerships/seniors/nhsp/faq.shtml
—————–. 2010a. Opportunities Fund: An Employment Program for Persons with Disabilities. Ottawa: HRSDC. Accessed June 28, 2011. https://www.hrsdc.gc.ca/eng/disability_issues/ funding_programs/opportunities_fund/ef.shtml
—————–. 2010b. Social Development Partnerships Program – Disability (SDPP-D). Ottawa: HRSDC. Accessed June 28, 2011. https://www.hrsdc.gc.ca/eng/community_partnerships/ sdpp/call/disability_component/page00.shtml
Keefe, J. Forthcoming. “Who Will Care for Older Canadians? Caregiving Policy Challenges in the Short and Long Terms.” IRPP Study. Montreal: Institute for Research on Public Policy.
Kent, T. 1988. A Public Purpose. Montreal and Kingston: McGill- Queen’s University Press.
Kershaw, P. 2002. “Beyond the Spousal Tax Credit: Rethinking Taxation of Dependency and Caregiving (Again!) in the Light of the Law Commission of Canada Report.” Canadian Tax Journal 50 (6).
LaRochelle-Côté, S., J. Myles, and G. Picot. 2008. Income Security and Stability in Canada during Retirement. Analytical Studies Branch Research Paper Series. Catalogue #11F0019M. Ottawa: Statistics Canada. Accessed January 5, 2010. https://www.statcan.gc.ca/pub/11f0019m/11f0019m2008306-eng.pdf
Lazar, H. 2006. “The Intergovernmental Dimension of the Social Union.” Canadian Public Administration 49 (1) 23-45.
Liberal Party of Canada. 2004. Moving Canada Forward: The Paul Martin Plan For Getting Things Done . Platform, 2004 elec- tion. Accessed November 1, 2011. https://www.cbc.ca/ canadavotes2004/pdfplatforms/Liberal_platform_en.pdf
Life Plans Inc. 1999. A Descriptive Analysis of Patterns of Informal and Formal Caregiving among Privately Insured and Non-pri- vately Insured Disabled Elders Living in the Community. Washington: US Department of Health and Human Services. Accessed February 19, 2010. https://aspe.hhs.gov/daltcp/ reports/ifpattrn.htm
MacDonald, B., D. Andrews, and R.L. Brown. 2009. “Basic Living Expenses for the Canadian Elderly.” Social and Economic Dimensions of an Aging Population Research Program, no. 240. Hamilton, ON: McMaster University.
MacKenzie, A., M. Hurst, and S. Crompton. 2009. Defining Disability in the Participation and Activity Limitation Survey. Living With Disability Series. Catalogue #11-008-X. Ottawa: Statistics Canada. Accessed January 23, 2010. https://bypass.wtnyein.co.cc/www.statcan.gc.ca/pub/11008- x/2009002/article/11024-eng.htm
Manitoba. 2010. Manitoba Finance. Primary Caregiver Tax Credit. Accessed June 28, 2011. https://www.gov.mb.ca/finance/tao/ caregiver.html
Margaret McGregor and Lisa A. Ronald. 2011. Residential Long- Term Care for Canada’s Seniors: Nonprofit, For-Profit or Does it Matter? IRPP Study 14. Montreal: Institute for Research on Public Policy.
National Union of Public and General Employees. 2007. Dignity Denied. Nepean, ON: NUPGE.
Noël, A. 2000a. “General Study of the Framework Agreement.” In The Canadian Social Union without Quebec, edited by A.-G. Gagnon and H. Segal. Montreal: Institute for Research on Public Policy.
—————–. 2000b. “Without Quebec: Collaborative Federalism with a Footnote?” Policy Matters 1 (2). Montreal: Institute for Research on Public Policy.
—————–. 2001. “Les prérogatives du pouvoir dans les relations intergouvernementales.” Enjeux Publics. Montreal: Institute for Research on Public Policy.
—————–. 2007. “L’union sociale revisitée.” Policy Options (March) Montreal: Institute for Research on Public Policy. IRPP Study, No. 23, September 2011
—————–. 2008. “Eliminer le pouvoir de dépenser.” Policy Options (March). Montreal: Institute for Research on Public Policy.
Nova Scotia. 2009. Department of Health. Allowance to Aid Caregivers. News release. Accessed June 28, 2011. https://www.gov.ns.ca/news/details.asp?id=20090811002
Ontario. 2011. Ministry of Health and Long-Term Care. Complex Continuing Care Co-payment 2010. Accessed June 28, 2011. https://www.health.gov.on.ca/english/public/pub/chronic/ch ronic.html
Osborne, J.E. 1985. The Evolution of the Canada Assistance Plan (Appendix to the Nielsen Task Force Report on the Canada Assistance Plan). Service to the Public — Canada Assistance Plan. Ottawa: Government of Canada. Accessed April 16, 2009. https://www.canadiansocialresearch.net/capjack.htm
Public Health Agency of Canada. 2006. Healthy Aging in Canada: A New Vision, a Vital Investment, from Evidence to Action — a Background Paper. A background paper prepared for the Federal, Provincial and Territorial Committee of Officials (Seniors). Ottawa: Public Health Agency of Canada.
Quebec. 1998. Quebec’s Historical Position on the Federal Spending Power: 1944-1998. Quebec City: SecreÌtariat aux Affaires intergouvernementales canadiennes.
Schellenberg, G., and Y. Ostrovsky. 2008. The Retirement Plans and Expectations of Older Workers. 2007 General Social Survey Report. Ottawa: Statistics Canada. Accessed August 28, 2011. https://www.statcan.gc.ca/pub/11-008-x/2008002/ article/10666-eng.htm#a3
Senate Standing Committee on Social Affairs, Science and Technology. 2002. The Health of Canadians — the Federal Role: Final Report. Ottawa: Parliament of Canada.
Social Union Framework Agreement. 1999. A Framework to Improve the Social Union for Canadians: An Agreement between the Government of Canada and the Governments of the Provinces and Territories, February 4, 1999. News release. N.p. Accessed February 24, 2010. https://www.socialunion.gc.ca/ news/020499_e.html
Statistics Canada. 2003. Disability Supports in Canada, 2001. Catalogue #89-590-XIE. Ottawa: Statistics Canada.
—————–. 2006a. Income in Canada 2006. Catalogue #75-202-X. Ottawa: Statistics Canada. Accessed January 6, 2010. https://www.statcan.gc.ca/pub/75-202-x/2006000/ 5203565eng.htm#tphp
—————–. 2006b. Net Worth of Family Units, by Selected Family Characteristics. Ottawa: Statistics Canada. Accessed February 25, 2010. https://www40.statcan.gc.ca/l01/cst01/famil112a- eng.htm
—————–. 2006c. Participation and Activity Limitation Survey 2006: Technical and Methodological Report. Catalogue #89-628-XIE. Ottawa: Statistics Canada.
—————–. 2008a. 2007 General Social Survey: Care Tables 2007, Table 3-1. Accessed August 28, 2011. https://www.statcan.gc.ca/pub/89-633-x/2008001/t018- eng.pdf
—————–. 2008b. Seniors. Ottawa: Statistics Canada. Accessed February 13, 2010. https://www41.statcan.gc.ca/2008/70000/ ceb70000_000-eng.htm
Statistics Canada. 2011. “Population Projections for Canada, Provinces and Territories 2009-2036.” Accessed November 1, 2011. https://www.statcan.gc.ca/bsolc/olc-cel/ olc-cel?catno=91-520-X&lang=eng
Taylor, M.G. 2009. Health Insurance and Canadian Public Policy. Carleton Library Series no. 213. 3rd ed. Montreal and Kingston: McGill-Queen’s University Press,
Torjman, S. 1997. Desperate for Respite. Ottawa: Caledon Institute for Social Policy.
Tremblay, A. 2000. “Federal Spending Power.” In The Canadian Social Union without Quebec, edited by A.-G. Gagnon and H. Segal. Montreal: Institute for Research on Public Policy.
Vaillancourt, Y. 2003. “The Quebec Model in Social Policy and Its Interface with Canada’s Social Union.” In Forging the Canadian Social Union: SUFA and Beyond, edited by S. Fortin, A. Noël, and St-Hilaire. Montreal: Institute for Research on Public Policy.
Wilkins, K. 2006. “Government-Subsidized Home Care.” Health Reports 17 (4). Catalogue #82-003. Ottawa: Statistics Canada. Accessed January 24, 2010. https://www.statcan.gc.ca/stud- ies-etudes/82-003/archive/2006/9497-eng.pdf
Wolfson, M. 2011. Projecting the Adequacy of Canadians’ Retirement Incomes: Current Prospects and Possible Reform Options. IRPP Study 17. Montreal: Institute for Research on Public Policy.
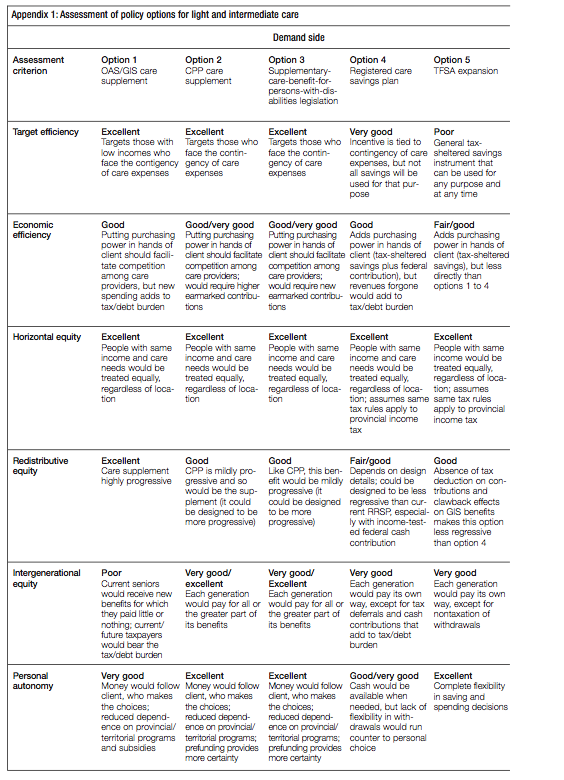
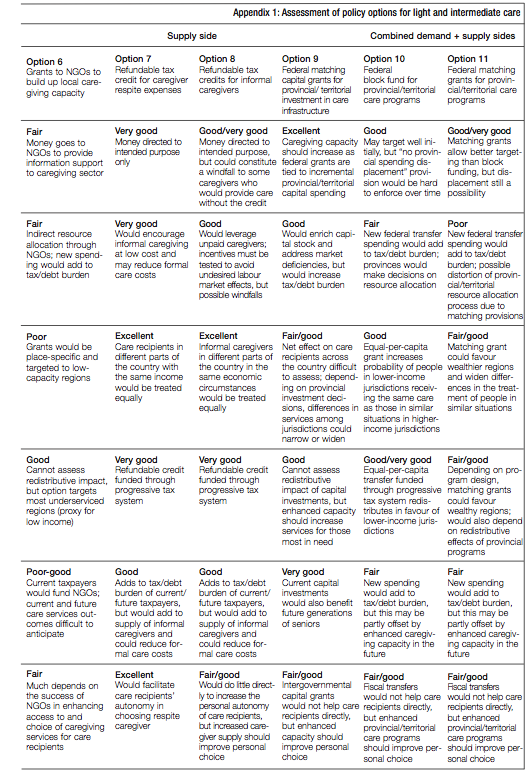
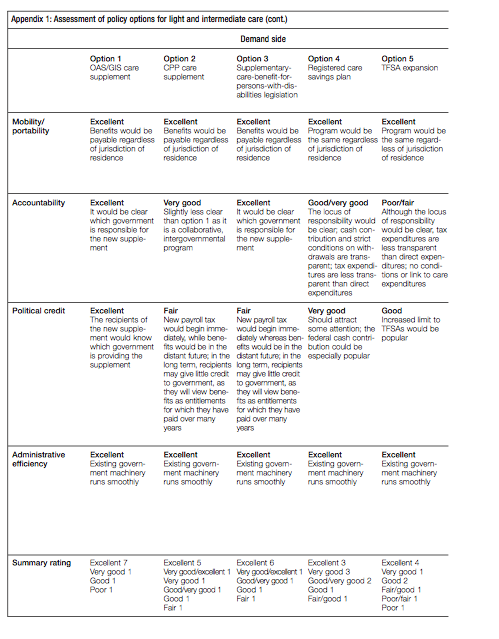
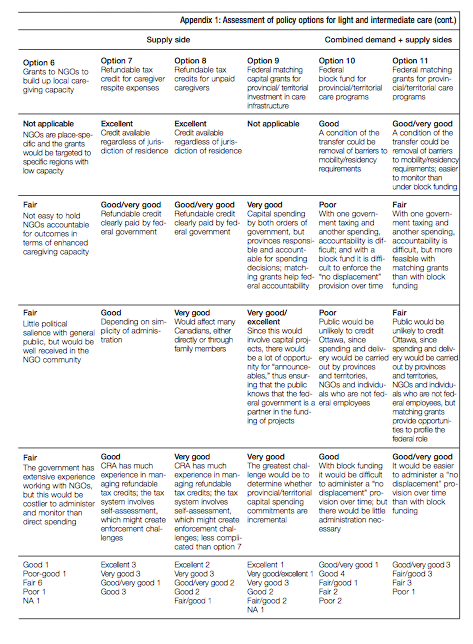
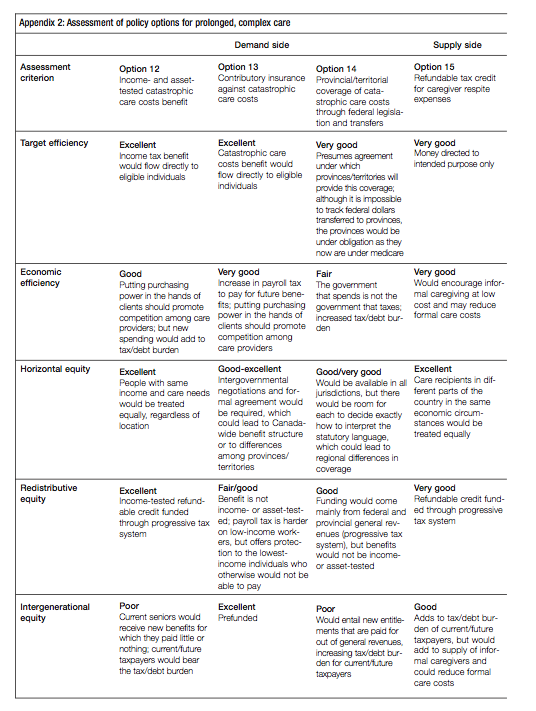
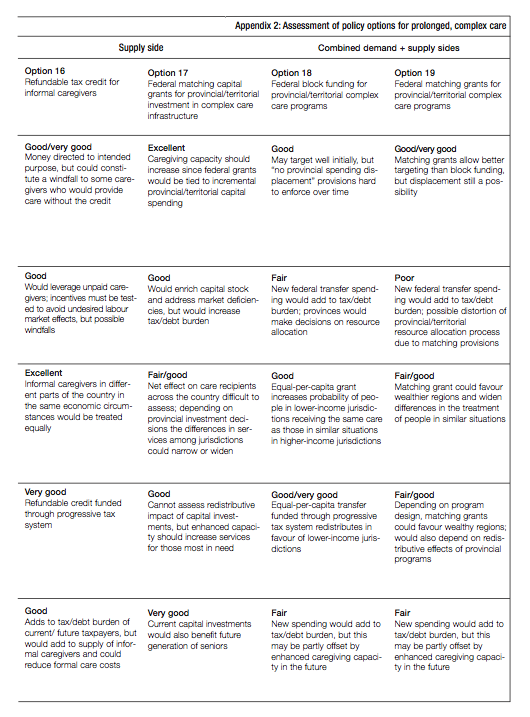
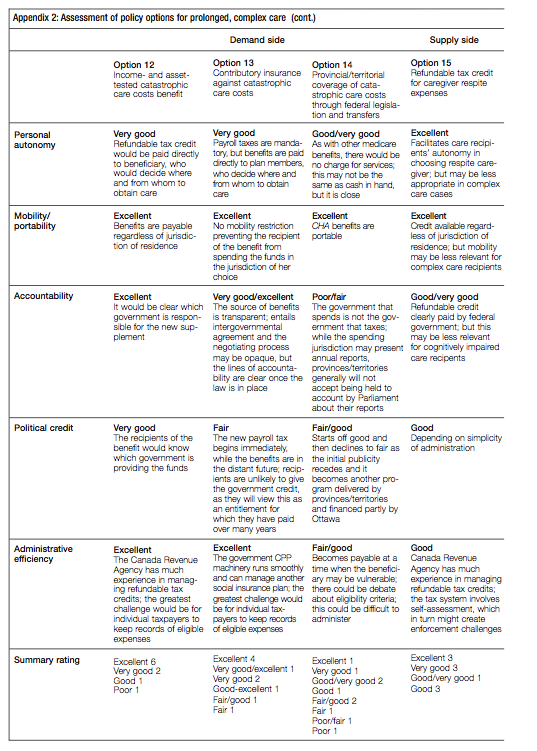
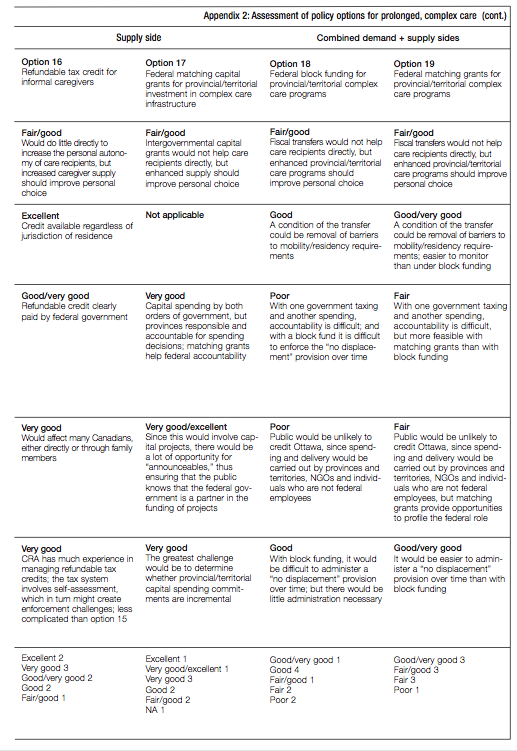
This publication was published as part of the Faces of Aging research program under the direction of Sarah Fortin and France St-Hilaire. The manuscript was copy-edited by Jane Broderick, proofreading was by Barbara Czarnecki, editorial coordination was by Francesca Worrall, production was by Chantal Létourneau, art direction was by Schumacher Design and printing was by AGL Graphiques.
Harvey Lazar is adjunct professor at the School of Public Administration and senior research associate at the Centre for Global Studies, University of Victoria. He spent much of his career in Ottawa. From 1997 to 2005 he was director of the Queen’s Institute of Intergovernmental Relations. He has edited or co-edited and co-authored nine volumes, including Spheres of Governance: Comparative Studies of Cities in Multilevel Governance Systems (2007); Canadian Fiscal Arrangements: What Works, What Might Work Better (2005); and Money, Politics and Health Care (2004). His current research is on health care reform in Canada.
To cite this document:
Lazar, Harvey. 2011. Many Degrees of Policy Freedom: The Federal Government’s Role in Care for Seniors. IRPP Study 24. Montreal: Institute for Research on Public Policy.
Although researchers have been warning of the aging of Canada’s population for decades, governments do not yet have an overarching policy strategy to deal with the profound, long-term socioeconomic implications of this demographic shift, let alone its more immediate impact on seniors’ care.
There is an imbalance between the demand for and supply of care for seniors and an expectation that this imbalance will grow. This expectation demands a public policy response. Part of that response is to decide « who does what » to improve the outlook. The federal government has a unique responsibility in helping Canadians decide who, in fact, will do what.
Ottawa plays the lead role in the provision of retirement income for seniors, both through the public pension system and the tax incentives it provides for employer-sponsored pensions and private savings. « Elderly benefits » are the federal government’s single largest expenditure category. Federal cash transfer payments to the provinces for health and social services are almost as large and have a significant influence on the availability and accessibility of seniors’ care.
With population aging, pension costs will grow, mounting pressures on the health-care system and care needs will climb. At the same time, the share of the population of labour force age will shrink.
Ottawa will be called upon to do more.
There are many actions that the federal government can take to address the growing and underfunded care needs of seniors without undermining the leadership role of the provinces, or assuming responsibility for activities that do not square with its view of how the fiscal side of the federation should be managed. There are, however, two initiatives that it must take which are essential for wise decision-making on this issue.
The federal government must commission a diagnosis of how well the care needs of seniors across the country are being satisfied today, with realistic projections of demand and supply at least a couple of decades into the future. Such an initiative is consistent with other recent decisions Ottawa has taken that demonstrate an interest in the medium and longerterm challenges of population aging.
First, by putting the age of entitlement for Old Age Security and related benefits into play, the prime minister has demonstrated a willingness to take a longterm view of the public interest.
Second, the fact that Finance Minister Jim Flaherty is moving forward with income-tax amendments to facilitate the creation of pooled pension plans shows a concern for the economic security of tomorrow’s seniors.
Third, recent government announcements of proposed changes to immigration-selection criteria shows a concern for the long-run capacity of the economy to bear the weight of an older population.
Sophisticated models can be used to assess pension reform options, both for age of entitlement and pooled pension plans. But here is the rub. These models do not contain basic information about the costs of care and its incidence.
There is a good argument to be made that there is a missing piece of our retirement-income system because it does not build in the probability of substantial care costs.
The federal government must use its resources to help shine some light on the facts. This task is scientific, not political. It should be assigned to a person or organization that is, and is seen to be, at arm’s length from government.
Given the stance that the federal government has taken on the renewal of the health accord, including public remarks by Prime Minister Stephen Harper, it is clear the Conservative government has no wish to occupy space that is the constitutional responsibility of the provinces. This proposal is compatible with that view of the federation. Indeed, it will not be possible to know if Ottawa is meeting its current constitutionally based leadership role on pensions without such a diagnosis.
The federal government must then inform Canadians how it interprets the population-aging challenges that lie ahead, what it plans to contribute and what it expects of others – individuals, the family unit, friends and neighbours, business, the social economy, as well as provincial and territorial governments.
There are in fact many degrees of freedom for the federal government to show leadership in seniors’ care without intruding on areas of exclusive provincial constitutional jurisdiction. Denying the responsibility to exercise this freedom would be one degree of freedom too many.
Harvey Lazar, author of the study Many Degrees of Policy Freedom: The Federal Government’s Role in Care for Seniors, is an adjunct professor at the School of Public Administration and senior research associate at the Centre for Global Studies, University of Victoria.
